Facial reconstruction after human bite injury
Garrison A Leach,1Jaclyn N Lundberg,1 and Travis C Holcombe2
Case presentation
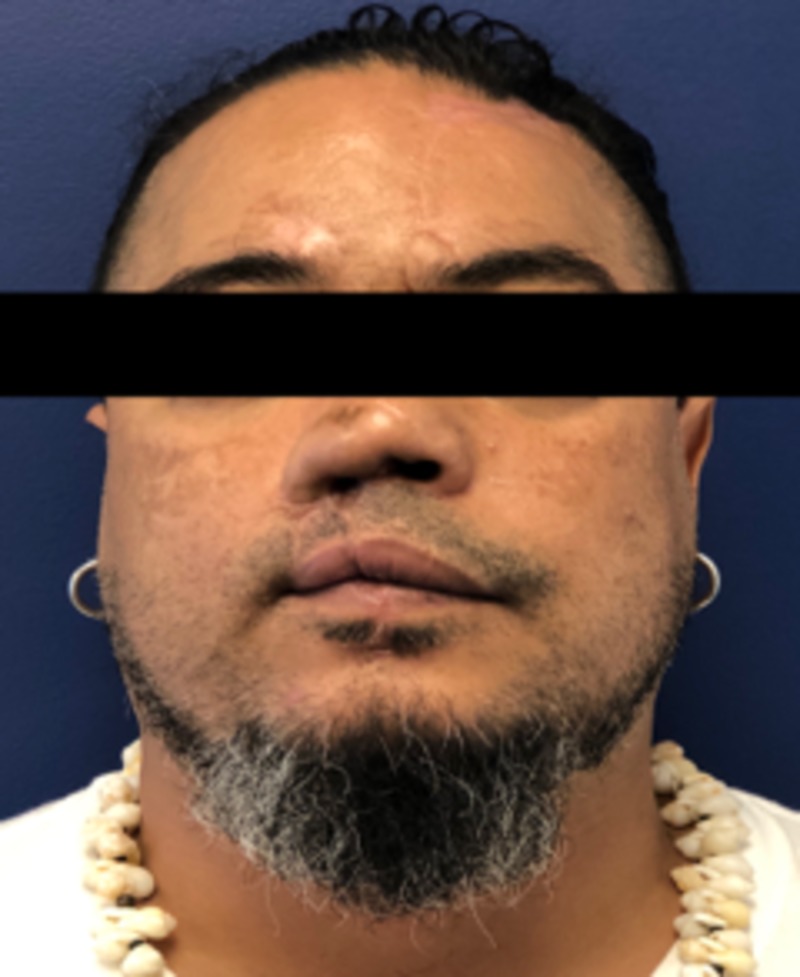
A 46-year-old male with a past medical history of hypertension presented to our trauma bay with complex injuries of the right nose and midface, which included an amputated nose, upper lip and right eyebrow approximately 40 minutes after an assault including numerous human bite wounds. His right ala, right sidewall, and right upper lip were entirely missing, with nasal airways on each side visible. The amputated specimens included nasal tissue which measured approximately 4.0 x 4.0 cm, the eyebrow 2.0 x 2.0 cm, and the upper lip 1.0 x 11.7 cm (Figure 1). After rapid sequence intubation, assessment, and stabilization, the patient was taken to the operating room about one hour after the initial presentation for reattachment and wound reconstruction.
In the OR, the superior labial artery and a small outflow vein, which was likely part of the superior labial venous plexus, were identified and isolated from the lateral portion of the lip. However, the nasal segment contained no identifiable viable artery or vein. Therefore, the nasal and eyebrow portions were replanted similarly to full thickness skin grafts and the upper lip was replanted using microvascular techniques. The segments of each vessel were flushed with heparinized saline. Then, the superior labial artery was anastomosed using 9-0 nylon interrupted sutures, followed by anastomosis of the vein using 9-0 nylon. After three hours and 19 minutes of operating time, arterial blood flow was immediately apparent, but venous flow was not definitive. The wounds of the upper eyelid and right cheek were debrided and then closed.
To improve the chance of tissue survival, our patient was scheduled to receive hyperbaric oxygen treatment within 24 hours post-operation. However, the patient reported that his ears could not tolerate the pressure and therapy was postponed until otolaryngology could insert tubes at the bedside. Additionally, he was receiving 30 mg of enoxaparin daily to mitigate the chance of outflow venous thrombosis. The replaced nasal and eyebrow tissue and the microsurgically replanted upper lip appeared to have some minor ischemia at the lateral margins (particularly of the nasal tip) that would most likely require revision, but the majority of the three portions appeared healthy (Figure 2).
Later that day, the patient reported upper extremity numbness. After a non-contrast CT showed no intracranial abnormality, he received 8.34 mg bolus of tPA followed by 75.1 mg of IV tPA over the course of an hour for possible ischemic stroke. Subsequent MRI showed a small acute left frontal cortical infarction. The next morning the patient reported chest discomfort and an EKG showed ST-segment elevation of inferior leads with elevated troponin peak of 132.2 due to myocardial infarction. The patient then underwent left heart catheterization that showed adequate flow and no need for further intervention. After these events, he received 30 mg of enoxaparin twice a day per protocol.
After tPA treatment, there was marked continuous sanguineous discharge from the replant sites and the eyebrow, nose, and upper lip began to appear increasingly dusky. Our patient was determined to be a high-risk candidate for immediate revision surgery and plans for secondary reconstruction were made. The patient returned six days later for facial wound debridement of necrotic wounds of the upper lip, nose, and right forehead with subsequent placement of Integra artificial dermis (Figure 3). He subsequently underwent nose and upper lip advancement flaps to save oral competence. A month later, nasal reconstruction was undertaken with a left paramedian forehead flap and full-thickness skin graft to upper lip and nose. The second stage of reconstruction was done one month later including the second stage of the paramedian flap, ear cartilage graft to the nose, and full-thickness skin graft of the upper lip (Figure 4). Subsequent reconstruction one month later included an Abbe flap from the lower lip to the upper lip and final revision of the forehead flap. Overall, our patient was satisfied with the cosmetic and functional outcome of his reconstruction four months after his final surgery (Figure 5).

Patient after the second stage of paramedian flap, ear cartilage graft to nose, and full-thickness skin graft of the upper lip, but prior to Abbe flap
Patient four months after final revision surgery
Author information
1 Surgery, Creighton University School of Medicine, Phoenix, USA
2 Plastic Surgery, Creighton University School of Medicine, Phoenix, USA
corresponding authorCorresponding author.
Garrison A. Leach
Human ethics
Consent was obtained by all participants in this study
References
References
- Survival of large replanted segment of upper lip and nose. Case report. James NJ. https://www.ncbi.nlm.nih.gov/pubmed/?term=Survival+of+large+replanted+segment+of+upper+lip+and+nose.+Case+report. Plast Reconstr Surg. 1976;58:623–625. [PubMed] [Google Scholar]
- Microvascular replantation of head and neck amputated parts: a systematic review. Efanov JI, Montoya IJ, Huang KN, Guertin C, Harris PG, Bou‐Merhi J, Danino AM. https://www.ncbi.nlm.nih.gov/pubmed/?term=Microvascular+replantation+of+head+and+neck+amputated+parts%3A+A+systematic+review. Microsurgery. 2017;37:699–706. [PubMed] [Google Scholar]
- Replantation of amputated facial tissues with microvascular anastomosis. Jeng SF, Wei FC, Noordhoff MS. https://www.ncbi.nlm.nih.gov/pubmed/7934800. Microsurgery. 1994;15:327–333. [PubMed] [Google Scholar]
- Lip replantation: a viable option for lower lip reconstruction after human bites, a literature review and proposed management algorithm. Liliav B, Zaluzec R, Hassid VJ, Ramasastry S, Kalimuthu R. https://www.ncbi.nlm.nih.gov/pubmed/?term=Lip+replantation%3A+a+viable+option+for+lower+lip+reconstruction+after+human+bites%2C+a+literature+review+and+proposed+management+algorithm J Plast Reconstr Aesth Surg. 2012;65:197–199. [PubMed] [Google Scholar]
- Successful replantation of an bitten-off lower lip: case report. Wong SS, Wang ML. https://www.ncbi.nlm.nih.gov/pubmed/10498327 J Trauma Acute Care Surg. 1999;47:602–604. [PubMed] [Google Scholar]
- Microvascular replantation of the avulsed lip. Godfrey ND, Akyurek M. https://insights.ovid.com/pubmed?pmid=30192293. J Craniofac Surg. 2018;29:717–720. [PubMed] [Google Scholar]
- Microsurgical replantation of the lip: a multi-institutional experience. Walton RL, Beahm EK, Brown RE, et al. https://www.ncbi.nlm.nih.gov/pubmed/?term=Microsurgical+replantation+of+the+lip%3A+a+multi-institutional+experience. Plast Reconstr Surg. 1998;102:358–368. [PubMed] [Google Scholar]
- Microvascular replantation following facial dog bites in children: systematic review and management algorithm. Williams AJ, Powers JM, Rhodes JL, Pozez AL. https://insights.ovid.com/pubmed?pmid=29762453. Ann Plast Surg. 2018;81:106–112. [PubMed] [Google Scholar]
- Microsurgical replantation of completely avulsed nasal segment. Akyurek M, Perry D. https://insights.ovid.com/pubmed?pmid=30507868. J Craniofac Surg. 2019;30:208–210. [PubMed] [Google Scholar]
- Management of perioperative microvascular thrombotic complications-The use of multiagent anticoagulation algorithm in 395 consecutive free flaps. Senchenkov A, Lemaine V, Tran NV. https://www.jprasurg.com/article/S1748-6815(15)00233-8/fulltext J Plast Reconstr Aesth Surg. 2015;68:1293–1303. [PubMed] [Google Scholar]
- Identification of independent risk factors for flap failure: a retrospective analysis of 1530 free flaps for breast, head and neck and extremity reconstruction. Las DE, de Jong T, Zuidam JM, Verweij NM, Hovius SE, Mureau MA. https://www.jprasurg.com/article/S1748-6815(16)00073-5/fulltext J Plast Reconstr Aesth Surg. 2016;69:894–906. [PubMed] [Google Scholar]
- Composite grafting and hyperbaric oxygen therapy in pediatric nasal tip reconstruction after avulsive dog-bite injury. Rapley JH, Lawrence WT, WittPD WittPD. https://www.ncbi.nlm.nih.gov/pubmed/?term=Composite+grafting+and+hyperbaric+oxygen+therapy+in+pediatric+nasal+tip+reconstruction+after+avulsive+dog-bite+injury. Ann Plast Surg. 2001;46:434–438. [PubMed] [Google Scholar]
- Microsurgically aided upper lip replantation-case report and literature review. Gustafsson J, Lidén M, Thorarinsson A. https://www.ncbi.nlm.nih.gov/pubmed/?term=Microsurgically+aided+upper+lip+replantation-case+report+and+literature+review. Case Reports Plast Surg Hand Surg. 2016;3:66–69. [PMC free article] [PubMed] [Google Scholar]
- Tissue plasminogen activator as an antiangiogenic agent in experimental corneal neovascularization in rabbits. Arai K, Yasukawa T, Kato A, et al. https://www.karger.com/Article/Abstract/487054. Ophthalmic Res. 2018;59:170–175. [PubMed] [Google Scholar]
- Tissue plasminogen activator as an antiangiogenic agent in experimental laser-induced choroidal neovascularization in mice. Ozone D, Mizutani T, Nozaki M, et al. https://www-ncbi-nlm-nih-gov.cuhsl.creighton.edu/pubmed/27727399. Invest Ophthalmol Vis Sc. 2016;57:5348–5354. [PubMed] [Google Scholar]
Articles from Cureus are provided here courtesy of Cureus Inc.


