Rotationplasty of the Left Leg Due to Severe Burn Contractures in a Patient with Contralateral Amputated Right Femur: A Case Report
1. Background
Van Nes Rotationplasty (VNPR) is a surgical procedure consisting of limb-saving shortening of the leg with a rotation of 180o of the lower leg which is adapted to the remaining femur, changing the ankle function into a new knee joint [1]. The functional outcome of such a technique is that the knee flexion corresponds to the former ankle dorsiflexion and the knee extension to the former ankle plantar flexion [2]. In order for this surgery to be performed the ankle should be in optimum condition prior to the procedure and the sciatic nerve should remain fully functional [3]. A prosthetic leg is worn for 6 weeks after the surgery to assist the patient with daily activities; the prosthesis contains a socket, a metal guided thigh shaft with a single – axis hinged joint at the upper ankle joint along with its lower part [4]. The extended position of the leg and the maximum flexion are controlled by the axis. This flexion ranges between 70° (in the beginning) and 90o, a limit which should not be surpassed to avoid a sprain or a fracture of the ankle. VNRP is a procedure that was originally used for several varieties of femur hypoplasia or absence [5], but had been also used in other forms lower limb deficiencies [2], trauma [6], tumors [3, 4, 7, 8], infected knee arthroplasty [9] and in one report was used in an extended burn around the knee [10]. When rotationplasty is applied, both the family and the patient should have the appropriate amount of information regarding the postoperative aesthetic outcome which can cause considerable psychological issues [2, 7, 8, 11] and it seems to be the only factor for which a rotationplasty is not usually selected as a treatment plan despite o its excellent results [12, 13]. Based on gait and electromyographic data, rotationplasty has proven to offer optimum, long-lasting gait rehabilitation [3]. The only deviations noticed concerning stride length, cadence, stride duration, stance – swing ratio and velocity were rather insignificant when compared to healthy people [12-15].
Case report
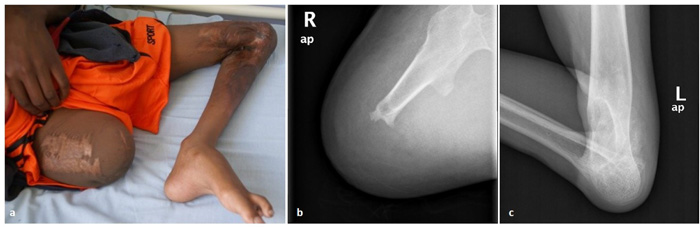
A 15-year-old boy from Tanzania was amputated on his right thigh (18 cm length from the hip joint) in his country 10 years ago after a severe burn injury that also left him with full contracture and extensive scar tissue deformities on the left knee. Scar skin extended from his left distal third of the thigh to the second third of his tibia (Fig. 1). For 10 years, the boy had never received rehabilitation or worn any prosthesis. He managed to move bearing mainly on his palms.
He was brought to our department by a non-profit organization (Tanzania Orphans Mission) seeking a solution that would allow him to walk again. Several options were considered: above knee amputation, progressive extension of the knee with the Ilizarov apparatus, endoprosthesis, intercalary strut graft and Van Nes Rotationplasty, which was finally chosen for reasons presented in the discussion section. The goal was to provide him with a functional ‘knee’ for later use of a prosthesis, similar to that used in below-knee amputees. The patient and his supporting friends gave their consent after they were fully informed about the pros and cons of this method, given special emphasis on the psychological effects.
Radiological depiction of the vascular network of the limb that was obtained preoperatively showed no considerable obstruction of the femoral artery and its branches. The operation lasted 3.5 hours. The neurovascular bundle was successfully released from the ample surrounding scar tissue and proximal tibia and distal femur were excised as much as enough for the remaining muscles to cover the bones. The required rotation (180 degrees) was easily achieved. We did not concern about the level of the new “knee” because the other knee did not exist either. The rest surgery was performed according to the original technique described by Van Nes. Split thickness skin graft was used to cover a defect in the middle of the surgical trauma. We needed to revise the trauma on the 6th postoperative day because the patient’s vital signs indicated consistent hemorrhage and the trauma site was progressively enlarged. A hole was found at the proximal part of the tibial artery that was successfully repaired. At the same time, additional split thickness skin graft was applied. The postoperative period was otherwise uncomplicated. The patient remained in the hospital for 1 month, where he started a daily rehabilitation program. Before his discharge, radiological examination showed early signs of callus formation and the patient was clear to wearing a prosthesis (Fig. 2).



After he left the hospital, we took measurements from the right limb for the fabrication of a prosthesis and an intense rehabilitation program was initiated. The specific problems that we had to deal with were the following: a) the right hip had a stiff contracture of 10° and muscle strength was reduced (MRC=3) which was not enough for the patient in order to use a prosthesis efficiently, b) the patient had not been in an upright position for 10 years, thus he had to relearn walking, c) the timeframe of rehabilitation had to be limited to 85 days because the patient had to get back to his country and also the fact that d) a double amputated patient demands much more effort and rehabilitation time. The physiotherapy treatment plan for the right (amputated) limb included complete strengthening in all levels, regaining full ROM in all movements and also efforts to release the contracture. For the left (VNRP) leg the goals were to regain muscle contraction after rotationplasty, 0° – 60° flexion extension ROM of the “new knee” and strengthening of the muscles that affect the flexion-extension movement of the “new knee” after regaining muscle contraction. In addition, we scheduled pulmonary physiotherapy, strengthening exercises of the upper limbs (to have the strength to use walking aids), and also of the abdominal and lumbar muscles. The details of the custom-made prostheses are described in Table 1. Non-dynamic knee and feet design was preferred because the patient’s condition required some movement restriction that provided better stability and control. However, the use of dynamic knee and feet mode is not excluded in the future, when the patient will be familiar with the use of his prostheses. Αn adapter with rotation was applied because in the beginning, the patient showed an inward rotation of the right stump, something that is expected to change in the future and consequently new alignment of the prosthesis can be made.
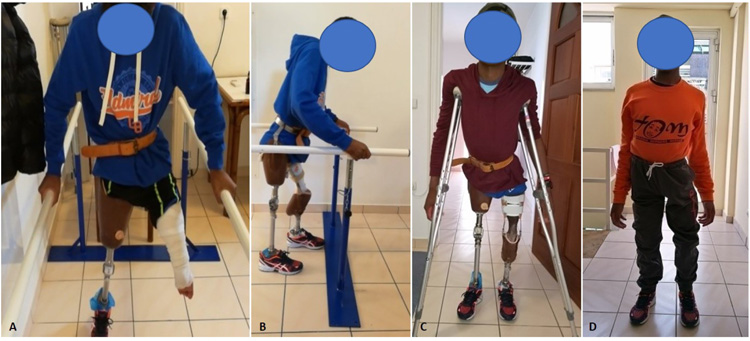
For the right stump, we started muscle strengthening on all muscle groups; initially the patient showed a score of 4 – in MRC scale on all movements of the thigh (flexion, extension, adduction, abduction) but with strengthening exercises and stretching we managed to increase the muscle strength to 5 in MRC scale in all movements and released the hip contracture in 15 days. At this point the prosthesis of the right limb was ready, and we started to train the patient on walking with one leg on a walkway with sidebars on both sides (Fig. 3A). After 10 days of training with the prosthesis, the patient could use it easily.
For the left thigh, we started muscle strengthening on all muscle groups which scored 3 in MRC scale in all movements of the thigh (flexion, extension, adduction, abduction). We also chose to use Low-frequency Pulsed Electromagnetic Fields (PEMF) (duration 40 mins / 4 times per week) at the compound point (femur with tibia) to reduce postoperative edema; this had probably a positive effect on bone healing as has been reported in recent studies [16, 17]. We excluded electrotherapy due to the hypersensitivity that the patient had around that area. We also used Visual Analog Scale (VAS) to assess pain taking care not to exceed a score of 6 during the whole rehabilitation process. At 20 days we got active ROM on all four levels and muscle strength score of 4- in MRC scale.
As for the ankle joint that had to function as a knee, passive ROM 0° – 65° but no active ROM was recorded from the first day of the rehabilitation. Strengthening exercises and stretching was initiated. At 18 days passive ROM was 0° – 90°. On the 22nd day the patient appeared to have a muscle strength score of 1 in MRC scale for the first time, gradually increased to 3 and 4- on the 32nd day and 45th day respectively. On the 58th day the muscle strength score was 4 in MRC scale and active ROM was 0° – 70°; at that time the second prosthesis for the left leg was applied and it was the first time after 10 years that the patient stood upright. Consequently, the patient began training on walking, with the prostheses applied on both legs, on a walkway with sidebars on both sides (Fig. 3B). Immediately after that, we added balance and stamina exercises. On the 65th day, the patient was able to use the two prostheses safely inside the walkway with sidebars and started walking with crutches (Fig. 3C). On the 75th day the patient could move and serve himself independently with the use of crutches and finally, on the 85th day, the day before his departure, the patient had muscle strength score 5 in MRC scale in flexion, extension, adduction and abduction in the right leg. At the left thigh he had full active ROM and muscle strength score 4+ in MRC scale in flexion, extension, adduction and abduction, and active ROM of 0° – 75° in flexion and extension of his “new knee” with muscle strength score 4+ in MRC scale in these two movements. On the 86th day the patient left for his country, happy and without hesitations about the aesthetic part of the rotationplasty (Fig. 3D).
Authors
Minos Tyllianakis, Andreas Panagopoulos*, Konstantinos Fokas, Argyriadi Eleni, Panagiotis Megas
Orthopaedic Department, Patras University Hospital, Patras, Greece
Original source
References
| [1] | Wick JM, Alexander KM. Rotationplasty – a unique surgical procedure with a functional outcome. AORN J 2006; 84(2): 189-214. CrossRefPubMed |
| [2] | Sakkers R, van Wijk I. Amputation and rotationplasty in children with limb deficiencies: Current concepts. J Child Orthop 2016; 10(6): 619-26. CrossRefPubMed |
| [3] | Hillmann A, Rosenbaum D, Schröter J, Gosheger G, Hoffmann C, Winkelmann W. Electromyographic and gait analysis of forty-three patients after rotationplasty. J Bone Joint Surg Am 2000; 82(2): 187-96. CrossRefPubMed |
| [4] | So NF, Andrews KL, Anderson K, et al. Prosthetic fitting after rotationplasty of the knee. Am J Phys Med Rehabil 2014; 93(4): 328-34. CrossRefPubMed |
| [5] | Van Nes CP. Rotation-plasty for congenital defects of the femur: Making use of the ankle of the shortened limb to control the knee joint of the prosthesis. J Bone Joint Surg Br 1950; 32: 12-6. CrossRef |
| [6] | Klos K, Mückley T, Gras F, Hofmann GO, Schmidt R. Early posttraumatic rotationplasty after severe degloving and soft tissue avulsion injury: A case report. J Orthop Trauma 2010; 24(2): e1-5. CrossRefPubMed |
| [7] | Forni C, Gaudenzi N, Zoli M, et al. Living with rotationplasty–quality of life in rotationplasty patients from childhood to adulthood. J Surg Oncol 2012; 105(4): 331-6. CrossRefPubMed |
| [8] | Rödl RW, Pohlmann U, Gosheger G, Lindner NJ, Winkelmann W. Rotationplasty – quality of life after 10 years in 22 patients. Acta Orthop Scand 2002; 73(1): 85-8. CrossRefPubMed |
| [9] | Dumont CE, Schuster AJ, Freslier-Bossa M. Borggreve-Van Nes rotationplasty for infected knee arthroplasty – A case report. Acta Orthop 2010; 81(2): 268-70. CrossRefPubMed |
| [10] | Khatri B, Richard B. Use of Van Nes rotationplasty to manage a burnt knee. Burns 2000; 26(1): 88-91. CrossRefPubMed |
| [11] | Benedetti MG, Okita Y, Recubini E, Mariani E, Leardini A, Manfrini M. How much clinical and functional impairment do children treated with knee rotationplasty experience in adulthood? Clin Orthop Relat Res 2016; 474(4): 995-1004. CrossRefPubMed |
| [12] | Rota V, Benedetti MG, Okita Y, Manfrini M, Tesio L. Knee rotationplasty: Motion of the body centre of mass during walking. Int J Rehabil Res 2016; 39(4): 346-53. CrossRefPubMed |
| [13] | Fuchs B, Sim FH. Rotationplasty about the knee: Surgical technique and anatomical considerations. Clin Anat 2004; 17(4): 345-53. CrossRefPubMed |
| [14] | Gebert C, Hardes J, Vieth V, Hillmann A, Winkelmann W, Gosheger G. The effect of rotationplasty on the ankle joint: Long-term results. Prosthet Orthot Int 2006; 30(3): 316-23. CrossRefPubMed |
| [15] | Ginsberg JP, Rai SN, Carlson CA, et al. A comparative analysis of functional outcomes in adolescents and young adults with lower-extremity bone sarcoma. Pediatr Blood Cancer 2007; 49(7): 964-9. CrossRefPubMed |
| [16] | Ross CL, Siriwardane M, Almeida-Porada G, et al. The effect of low-frequency electromagnetic field on human bone marrow stem/progenitor cell differentiation. Stem Cell Res (Amst) 2015; 15(1): 96-108. CrossRefPubMed |
| [17] | Putowski M, Piróg M, Podgórniak M, et al. The use of electromagnetic radiation in the physiotherapy. European Journal of Medical Technologies 2016; 2: 53-8. |
Copyright
© 2019 Tyllianakis et al.
Open-Access License: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.