Fatal Facial Firework Injury
Patient is a 30-year-old male who presented to the ED from the field with extensive facial trauma secondary to a firework blast to the face. His airway was secured immediately upon arrival due to an altered mental status with a GCS of 3 and poor oxygenation. A glidescope intubation with a size 7 tube was performed, with almost immediate replacement of a size 8 tube when an air leak was found. Exchange of the endotracheal tube was guided with the help of a bougie. He was hypotensive initially and had episodes of bradycardia. The hypotension responded to fluids. He had extensive facial blast injury with a large amount of tissue loss of the eyes, forehead and nose (Figure 2). Both of the eyes were clinically ruptured. The maxilla was unstable upon examination. Focused assessment with sonography for trauma was performed and no free fluid was found. Ophthalmology, neurosurgery, and plastic surgery services were consulted.
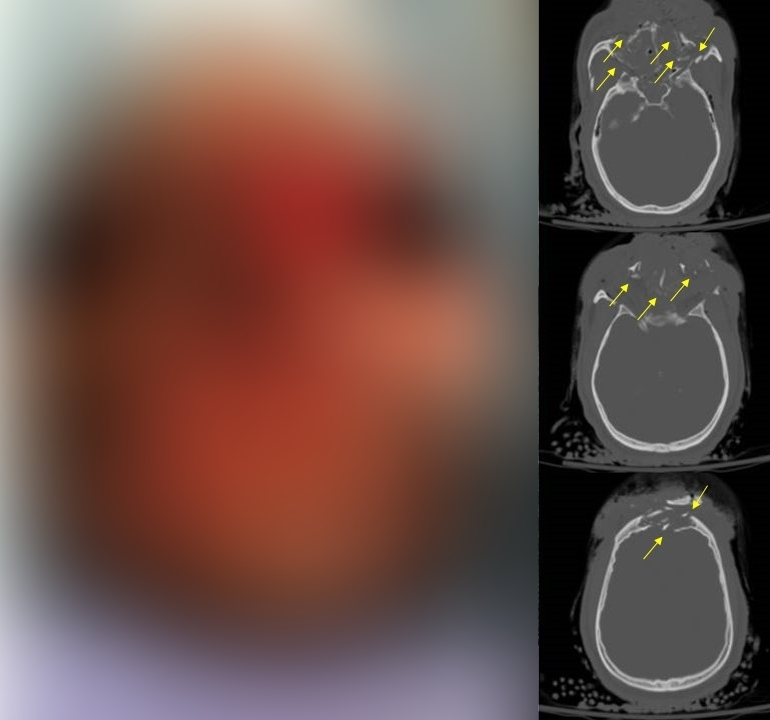
CT head revealed diffuse cerebral edema with effacement of the 3rd and 4th ventricles, subarachnoid hemorrhage and bilateral frontal and temporal contusions. CT maxillofacial revealed multiple complex fractures as follows: frontal bone with a comminuted fracture involving the inner and outer table and displacement of both; large defect noted in the anterior and central skull base with destruction of the ethmoid complex and the sphenoid bone; left temporal bone fracture with involvement of the inner ear and mastoid sinus; bilateral orbital, pterygoid, zygomatic and maxillary sinus fractures; fracture of the hard palate with obvious diastases of the bone fragments; and a mandibular body fracture. In addition the CT of the face revealed bilateral globe ruptures with extensive edema of the ophthalmic nerves and extraocular muscles.
The patient was admitted to the ICU. Consultation of neurosurgery, ophthalmology and plastic surgery were obtained. Post injury the patient developed persistent high fevers and was treated with antibiotics, he developed central diabetes insipidus, and was minimally responsive with only a cough and a gag. Eventually he was able to intermittently move his upper and lower extremities with stimulus. No surgical intervention was planned for his injuries.
On hospital day six, the patient underwent tracheostomy, percutaneous endoscopic gastrostomy tube placement, and facial wound debridement, all of which were uneventful. On hospital day seven, the patient had an increasing pressor requirement and fevers. His responsiveness also diminished after the operating room and it was thought that he progressed to brain death. He was in the middle of a brain death workup when he went into cardiac arrest. After 3 cycles of cardiopulmonary resuscitation, the patient was pronounced dead.