Above-the-knee replantation in a child: a case report with a 24-year follow-up
On April 23, 1986, a 3-year-old girl was brought to our institution after a 1.5-ton truck ran over her left lower limb. She suffered a floating knee injury with fractures at the supracondylar level of the femur and middle third of the tibia. An above the knee and near-total amputation was sustained at the supracondylar level, with a complete degloving of the thigh up to the inguinal area (Fig. 1). There were no other injuries.

Replantation started at 9 h after injury. The supracondylar fracture was fixed with Kirschner wires, followed by intramedullary nailing of the tibial fracture using a Steinmann pin. The popliteal artery was anastomosed using a 5-cm vein graft from the contralateral saphenous vein after which two popliteal vein anastomoses were performed. The peroneal and tibial nerves were then repaired followed by repair of the quadriceps femoris, hamstrings and triceps surae. The degloved skin was defatted and was re-applied as a full-thickness skin graft to the thigh.
The patient was stable postoperatively. A few days after surgery, skin and muscle necrosis of the gastroc-soleus complex developed, requiring repeated debridement before a split-thickness skin graft could be applied (Fig. 2). Two months after the index surgery, the patient had begun rehabilitation exercises for the lower extremity. After removal of the Steinman pin, an anteromedial external fixator was applied for two and a half months on the tibia in order to facilitate range of motion and weight-bearing exercises. The patient was discharged 1 month later.

At 4 years after the injury, the patient was ambulatory without assistance and no leg length discrepancy was noted at the time; knee flexion was noted at more than 90° and ankle dorsiflexion was to 10°. Six years after injury, the patient was able to stand on the affected limb without support, but soft tissue contractures had developed in the ankle and knee joints. No intervention was done at this time. When patient was 11 years old, 8 years after the injury, the knee flexion contracture was severe and a Z-plasty of the popliteal area to release the scar tissue contracture (Fig. 3) was carried out. With continued rehabilitation, the patient was able to regain full knee extension though flexion was limited to 90°. She was ambulatory without support but left with an equinus deformity of the left ankle. The leg length discrepancy had become more pronounced at this time of a growth spurt. She underwent her last major surgery when she was 12 years old; a femoral osteotomy was done, and an external fixator was applied for gradual lengthening to correct the 6-cm shortening of the left lower extremity.
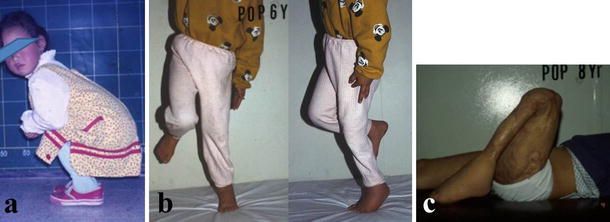
At the last review in September 2009, the patient was 25 years old. At 21 years after the incident, she remained freely ambulatory but with an equinus deformity of the left ankle. The knee range of motion was maintained at 0–90 degrees of flexion, the foot was sensate, and she was also able to move her toes (Fig. 4). Radiographs taken showed left lower extremity was shorter but the fractures and osteotomy sites had completely remodeled (Fig. 5). In 2012 through a telephone interview, the patient described her knee movement as unchanged and had no new complaints. She was satisfied with the functional outcome of her left lower limb despite it not being esthetically pleasing. Aside from the operative scars from the skin grafts, the limb was thinner from severe reduction in muscle bulk over the leg where debridement had been done. The patient was content that she was walking with her own limb with intact sensation and had avoided a prosthesis.
