A Novel Method for Retention of an Orbital Prosthesis in a Case with Continuous Maxillary and Orbital Defect
Gunjan Pruthi,1Veena Jain,2 and Swati Sikka3
Case Report
A 55-year-old male patient had reported to the Department of Prosthodontics, AIIMS, with a chief complaint of missing right eye since 3 months and regurgitation of food from the defect site. Patient gave the history of diabetes and histopathological diagnosis revealed Rhinocerebral mucormycosis. Surgical exenteration of the right eye and right side hemimaxillectomy was done to treat Rhinocerebral mucormycosis, and was followed by protocol of maintenance chemotherapy. Extraoral examination of the patient showed a large orbital defect on right side which was continuous with intraoral maxillary defect (Fig. 1). Extra orally, tissue was healthy but no definite bony or soft tissue undercut was found to help in the retention of the prosthesis. For complete prosthetic rehabilitation of the patient, a hollow closed bulb obturator and a silicone orbital prosthesis were planned. As the intraoral and extraoral defects were continuous, so to retain the orbital prosthesis, it was plugged with the help of pin of electric plug into the socket attached to the bulb of maxillary obturator (like a patrix and matrix).

Orbital defect continuous with intraoral maxillary defect
Method
Recording the Impressions
The patient was draped for impression procedures and patient’s eyebrows and eyelashes were lubricated with petroleum jelly in order to facilitate removal of the impression material and minimize discomfort to the patient. Lines were marked on the patient’s face with an indelible pencil for symmetrical placement of the orbital prosthesis. Impressions of the orbital defect and the maxillary defect were made using irreversible hydrocolloid (Zelgan, Dentsply India Ltd.) and individual casts were poured in dental stone for better surface details and strength.
Fabrication of Conformer and Attachment of Pin and Socket
A conformer of orbital defect was made with the autopolymerising resin (DPI cold cure, Dental Product of India, Mumbai, India) and was tried on patients face. A 5 mm thick sprue wax was attached to the acrylic base to provide a mechanical undercut for the retention of silicone eye prosthesis. An obturator plate was also made in cold cure acrylic resin and adjusted in patient’s mouth. A pin of electric plug was attached on the rear side of the conformer and a corresponding socket pin was attached to the bulb of the maxillary obturator plate. Both parts were snuggly fitted into each other like a matrix and patrix part of a semi precision attachment and adjusted to attain a path of insertion and removal without interference, so that the orbital prosthesis could be retained with the obturator in the absence of anatomic undercuts. The pin and socket were stabilized with sticky wax to the acrylic conformer and obturator plate, respectively. Conformer and obturator plate were flasked and dewaxed and packing was done in heat cure acrylic resin (high impact heat cure acrylic, Travelon) (Fig. 2). Pigments were added to the resin used for packing of orbital defect to match the patient’s skin color. The heat cure bases were checked on the patient for the adaptation and retentive potential (Fig. 3).

Flasking of acrylic base

Try-in of acrylic base on patients face
Fabrication of Silicone Orbital Prosthesis
The right eye prosthesis was carved in modeling wax using a prefabricated eye shell button selected according to the color of the left eye. It was tried on the patient’s face to check the orientation of pupil, color, size and volume of sclera visible as compared to the contra lateral eye. Once the trial was found satisfactory, flasking, dewaxing and packing were done as per Prosthodontic protocols and processed in RTV (room temperature vulcanizing) silicone material. Silicone-specific colors were used to match the color of the patient’s skin. Try-in of definitive obturator was done. It was flasked in a conventional manner and was delivered to the patient after finishing and polishing (Fig. 4a, b). Eye prosthesis was retrieved, characterized and was delivered to the patient (Figs. 5, ,6).6). Patient could wear the prosthesis with or without spectacle (Figs. 7, ,8).
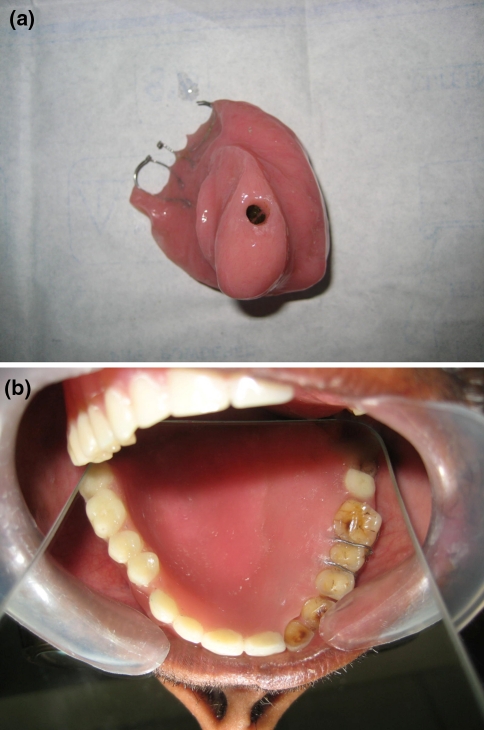
a Definitive obturator with socket pin. b Intraoral view of definitive obturator
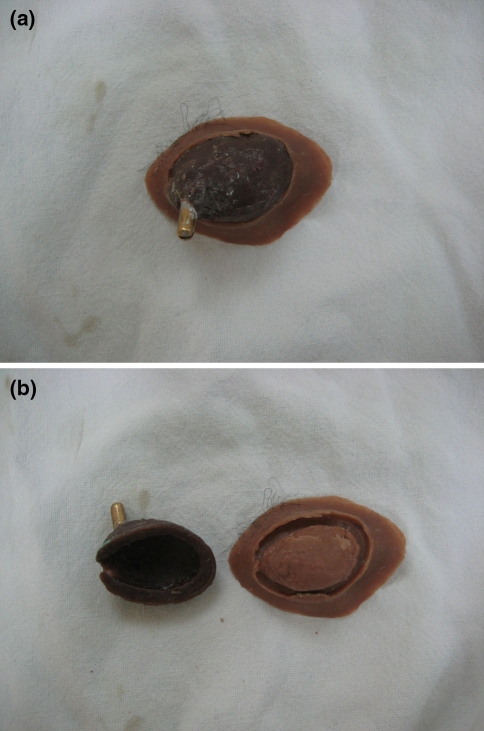
a Orbital prosthesis with socket pin. b Acrylic conformer and silicone prosthesis

Final eye prosthesis

Final prosthesis on patients face with spectacle

Final prosthesis on patients face without spectacle
Author information
All India Institute of Medical Sciences, New Delhi, 110029 India
2Department of Prosthodontics, All India Institute of Medical Sciences, New Delhi, 110029 India
3Department of Prosthodontics, Center for Dental Education and Research, All India Institute of Medical Sciences, 2nd floor, New Delhi, 110029 India
Gunjan Pruthi,
References
References
- Brignoni R, Dominici JT. An intraoral–extraoral combination prosthesis using an intermediate framework and magnets: a clinical report. J Prosthet Dent. 2001;85:7–11. doi: 10.1067/mpr.2001.113030. [PubMed] [CrossRef] [Google Scholar]
- Dhiman R, Arora V, Kotwal N. Rehabilitation of a Rhinocerebral mucormycosis patient. J Indian Prosthodont Soc. 2007;7:88–91. doi: 10.4103/0972-4052.34003. [CrossRef] [Google Scholar]
- Tautin FS, Schoemann D. Retaining a large facial prosthesis. J Prosthet Dent. 1975;34:342–345. doi: 10.1016/0022-3913(75)90115-8. [PubMed] [CrossRef] [Google Scholar]
- McClelland RC. Facial prosthesis following radical maxillofacial surgery. J Prosthet Dent. 1977;38:327–330. doi: 10.1016/0022-3913(77)90310-9. [PubMed] [CrossRef] [Google Scholar]
- Fattore L, Edmonds DC. A technique for the obturation of anterior maxillary defects with accompanying midfacial tissue loss. J Prosthet Dent. 1987;58:203–205. doi: 10.1016/0022-3913(87)90177-6. [PubMed] [CrossRef] [Google Scholar]
- Dumbrigue HB, Fyler A. Minimizing prosthesis movement in a midfacial defect: a clinical report. J Prosthet Dent. 1997;78:341–345. doi: 10.1016/S0022-3913(97)70040-4. [PubMed] [CrossRef] [Google Scholar]
- Amnuay SK, Khan Z, Goldsmith LJ. Effect of adhesive retention on maxillofacial prostheses. Part I: skin dressings and solvent removers. J Prosthet Dent. 2000;84:335–340. doi: 10.1067/mpr.2000.109507. [PubMed] [CrossRef] [Google Scholar]
- Wolfaardt JF, Tam V, Faulkner MG, Prasad N. Mechanical behavior of three maxillofacial prosthetic adhesive systems: a pilot project. J Prosthet Dent. 1992;68:943–949. doi: 10.1016/0022-3913(92)90556-P. [PubMed] [CrossRef] [Google Scholar]
- Parel SM. Diminishing dependence on adhesives for retention of facial prosthesis. J Prosthet Dent. 1980;43:552–560. doi: 10.1016/0022-3913(80)90330-3. [PubMed] [CrossRef] [Google Scholar]
- Chang TL, Garrett N, Roumanas E, Beumer J., III Treatment satisfaction with facial prosthesis. J Prosthet Dent. 2005;94:275–280. doi: 10.1016/j.prosdent.2005.06.002. [PubMed] [CrossRef] [Google Scholar]
- Nishimura RD, Roumanas E, Moy PK, Sugai T. Nasal defects and osseointegrated implants: UCLA Experience. J Prosthet Dent. 1996;76:597–602. doi: 10.1016/S0022-3913(96)90436-9. [PubMed] [CrossRef] [Google Scholar]
- Lemon JC, Chambers MS. Locking retentive attachment for an implant-retained auricular prosthesis. J Prosthet Dent. 2002;87:336–338. doi: 10.1067/mpr.2002.122016. [PubMed] [CrossRef] [Google Scholar]
- Arcuri M, LaVelle WE, Fyler E, Jons R. Prosthetic complications of extraoral implants. J Prosthet Dent. 1993;69:289–292. doi: 10.1016/0022-3913(93)90108-Z. [PubMed] [CrossRef] [Google Scholar]
- Konstantinidis L, Scolozzi P, Hamedani M. Rehabilitation of orbital cavity after total orbital exenteration using oculofacial prostheses anchored by osseointegrated dental implants posed as a one step surgical procedure. Klin Monbl Augenheilkd. 2006;223:400–404. doi: 10.1055/s-2006-926565. [PubMed] [CrossRef] [Google Scholar]
- Rodrigues S, Shenoy VK, Shenoy K. Prosthetic rehabilitation of a patient after partial rhinectomy: a clinical report. J Prosthet Dent. 2005;93:125–128. doi: 10.1016/j.prosdent.2004.10.021. [PubMed] [CrossRef] [Google Scholar]
- Guttal SS, Patil NP, Nadiger RK, et al. Use of acrylic resin base as an aid in retaining silicone orbital prosthesis. J Indian Prosthodont Soc. 2008;8:112–115. doi: 10.4103/0972-4052.43615. [CrossRef] [Google Scholar]
Articles from The Journal of the Indian Prosthodontic Society are provided here courtesy of Wolters Kluwer — Medknow Publications
Copyright and License
Copyright © Indian Prosthodontic Society 2010