Abscesses in the brain following teeth gum infection
We report the case of a 65-year-old man with a medical history of prostate carcinoma, for which he underwent radical prostatectomy with adjuvant radiotherapy. The patient also had type 2 diabetes, hypertension, hypercholesterolaemia and epilepsy of unknown origin during his childhood. Home medications included acetylsalicylic acid, olmesartan medoxomil, rosuvastatin, lixisenatide, metformin and gliclazide. The patient was previously treated with valproate, which was reduced and then stopped 6 months earlier as the patient was seizure free for over 20 years. Previous imaging reports never mentioned intracranial anomalies. Detailed findings and events are illustrated in the patient’s timeline (figure 1).
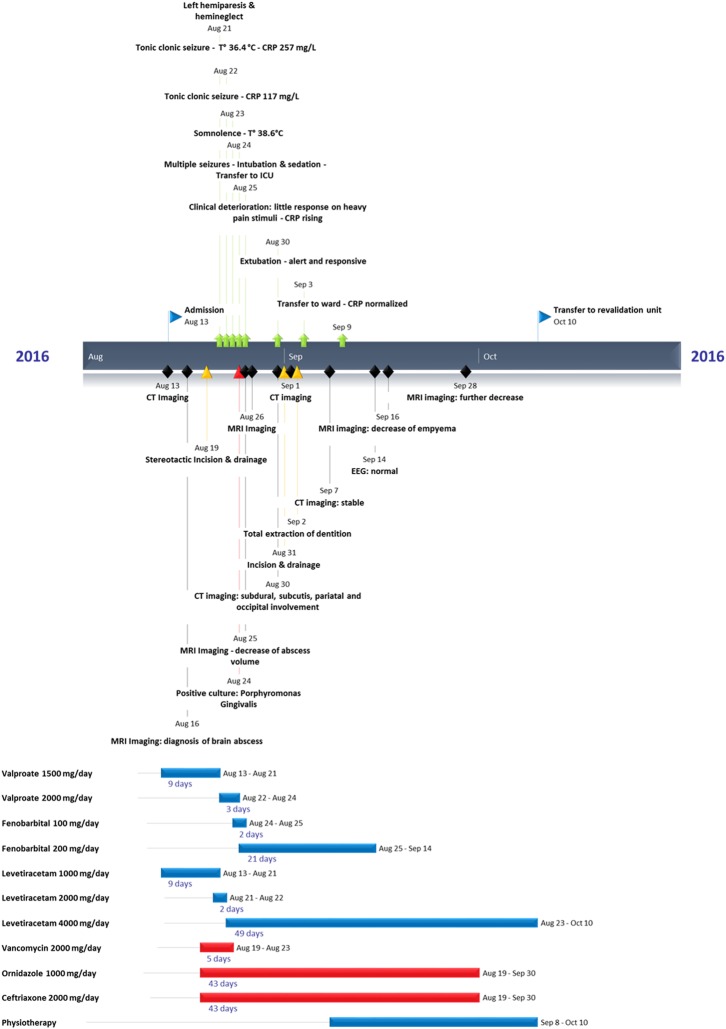
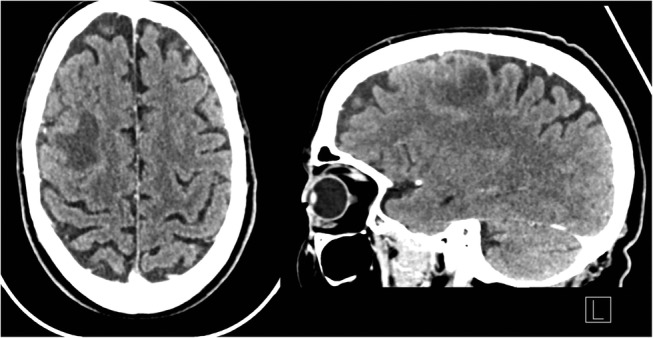
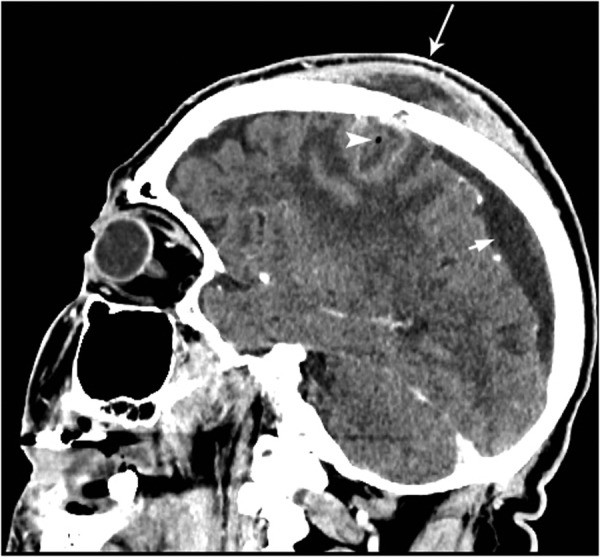
In August 2016, he was admitted after a generalised epileptic seizure at home. The patient’s wife reported that he was increasingly confused in the preceding days. The clinical neurological examination was normal with a Glasgow Coma scale (GCS) of 15/15. Blood tests were unremarkable except for a slightly increased C reactive protein (CRP) of 5.9 mg/L (reference <5.0 mg/L). An EEG was normal. A CT scan of the skull was performed showing a hypodense, contrast-enhanced lesion surrounded by oedema in the right frontal lobe (figure 2). No midline shift or ventricular anomalies were noted. An initial oncologic screening was advised with imaging of the chest and abdomen due to the medical history, but did not show primary malignancies or recurrence. After neurosurgical counsel, MRI with diffusion-weighted imaging (DWI) was added to the diagnostic workup and a brain abscess with pachymeningitis was diagnosed (figure 3, ). In light of these findings, a transthoracic ultrasound was negative for cardiac vegetations or signs of infection. Initial treatment consisted of systemic valproate (1.5 g/day), levetiracetam (1 g/day), vancomycin (2 g/day), ornidazole (1 g/day) and ceftriaxone (2 g/day). Stereotactic drainage was performed and MALDI-TOF spectrometry of the pus (Bruker Daltonik Maldi Biotyper) revealed P. gingivalis as the sole causative bacterium (score 2.231, high-confidence identification). Intraoral inspection showed partial dentition complicated with parodontitis. On previous CT imaging, apical periodontitis was seen around the elements 16, 23 and 34 (figure 4), and the sinus cavities appeared normal. The antibiotic regimen was reduced to intravenous ornidazole (1 g/day) and ceftriaxone (2 g/day).


Nineteen days after initial drainage, left hemiparesis and left hemineglect developed as well as an increase in epileptic seizures with one tonic–clonic seizure. The patient further deteriorated with need for intubation and intravenous sedation. Imaging showed the intracerebral abscess was extending to the subdural space and subcutis, forming a subdural empyema and spreading to the occipital–parietal regions; therefore, incision and drainage (figure 5) was necessary. Owing to clinical instability, total extraction of the remaining dentition was performed in a separate procedure. Antibiotic treatment included intravenous ceftriaxone (2 g/day) and ornidazole (1 g/day), which were continued for a total of 43 days until clinical, biochemical and radiological improvement. The patient was discharged from the neurosurgical ward after 59 days with almost complete resolution of the neurological deficit. He was referred for inhospital physiotherapy to regain full motor function.
Frederic Van der Cruyssen, Koenraad Grisar, Honorine Maes, and Constantinus Politis
OMFS-IMPATH Research Group, Department of Imaging and Pathology, Faculty of Medicine, Catholic University Leuven, Leuven, BelgiumCorrespondence to Dr Frederic Van der Cruyssen, eb.nevuelzu@nessyurcrednav.cirederf