Association Between the Level of Low-Density Lipoprotein Cholesterol and Coronary Atherosclerosis in Patients Who Have Undergone Coronary Computed Tomography Angiography
Abstract
Background
Although the Japan Atherosclerosis Society Guidelines 2017 recommend lower levels of low-density lipoprotein cholesterol (LDL-C, < 70 mg/dL or ≤ 100 mg/dL) to prevent secondary cardiovascular events, we cannot conclude that a low level of LDL-C prevents primary cardiovascular events in patients with suspected coronary artery disease (CAD).
Methods
We registered 1,016 patients who were clinically suspected to have CAD and who underwent coronary computed tomography angiography (CCTA) for screening of coronary atherosclerosis. We excluded 350 patients who were receiving anti-lipidemic therapies and finally analyzed 666 patients. The patients were divided into three groups according to the LDL-C level: < 70 mg/dL (n = 25, Low LDL-C), 70 – 99 mg/dL (n = 141, Middle LDL-C), and ≥ 100 mg/dL (n = 500, High LDL-C). A ≥ 50% coronary stenosis was initially diagnosed as CAD, and the number of significantly stenosed coronary vessels (VD), Gensini score and coronary artery calcification (CAC) score were quantified.
Results
There were no significant differences in age, high-density lipoprotein cholesterol, rates of hypertension, hemoglobin A1c, blood sugar or systolic blood pressure among the Low, Middle and High LDL-C groups. On the other hand, there were significant differences in rates of males, smoking, dyslipidemia and diabetes, diastolic blood pressure and triglyceride among the groups. The prevalence of CAD values in the Low, Middle and High LDL-C groups were similar, at 52%, 47%, and 46%, respectively. In addition, there were no significant differences in the number of VD, Gensini score or CAC score among the Low LDL-C, Middle LDL-C and High LDL-C groups.
Conclusions
We showed that the level of LDL-C was not associated with the presence or severity of CAD, which indicates that we need to screen by CCTA to prevent primary coronary events even if patients without anti-lipidemic therapies show low levels of LDL-C.Keywords: Low-density lipoprotein cholesterol, Coronary artery disease, Coronary computed tomography angiography, Gensini scoreGo to:
Introduction
The incidence of atherosclerotic cardiovascular disease (ASCVD) is high when low-density lipoprotein cholesterol (LDL-C) and/or triglyceride (TG) levels are high and/or when the high-density lipoprotein cholesterol (HDL-C) level is low [1–5]. According to the Japan Atherosclerosis Society Guidelines for the Prevention of Atherosclerotic Cardiovascular Diseases 2017 [6], the management target for LDL-C for primary prevention in patients with low, moderate and high coronary risk should be < 160 mg/dL, < 140 mg/dL and < 120 mg/dL, respectively. Moreover, the target LDL-C for secondary prevention in patients with a history of coronary artery disease (CAD) is < 100 mg/dL. For patients who have high-risk conditions, such as familial hypercholesterolemia, acute coronary syndrome or diabetes complicated by other high-risk conditions, the target LDL-C is < 70 mg/dL.
We have been studying the Coronary Computed Tomography Angiography (FU-CCTA) Registry at Fukuoka University in Japan and have identified coronary risk factors for the primary prevention of CAD [7–16]. In this Registry, none of the patients were diagnosed with CAD until the time of CCTA because we used CCTA to screen for CAD. When patients had significant coronary stenosis as assessed by CCTA, they were initially diagnosed with CAD.
Therefore, using the FU-CCTA Registry, we hypothesized that the target LDL-C level for primary prevention of coronary events in patients should be < 70 mg/dL or < 100 mg/dL.
Materials and Methods
Study subjects
One thousand sixteen consecutive subjects who were clinically suspected of having CAD or who had at least one cardiac risk factor (aging, gender male, hypertension (HTN), dyslipidemia (DL), diabetes mellitus (DM), smoking, obesity, family history of CAD and/or chronic kidney disease (CKD)) underwent CCTA. Suspected CAD is defined as having some chest symptoms and/or electrocardiogram (ECG) abnormalities. All subjects underwent CCTA between 2012 and 2019. Patients with creatinine > 2.0 mg/dL or contrast-induced allergy did not undergo multidetector computed tomography (MDCT). This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. The protocol in this study was approved by the ethics committee of Fukuoka University Hospital (#09-10-02), and all subjects gave their written informed consent to participate.
Evaluation of coronary stenosis using CCTA
We evaluated coronary stenosis using CCTA as previously described [7–9]. Patients were assessed by 64-MDCT on an Aquilion 64 (TOSHIBA, Tokyo, Japan) or by 320-MDCT on an Aquilion ONE ViSION (TOSHIBA, Tokyo, Japan). Overall, 15 coronary artery segments were assessed in all patients. Narrowing of the normal contrast-enhanced lumen to ≥ 50% that could be identified in multiplanar reconstructions or cross-sectional images was defined as significant stenosis [17]. The narrowing of the normal contrast-enhanced lumen to ≥ 70% was also defined as significant stenosis. When patients had significant coronary stenosis, they were initially diagnosed with CAD. In addition, in all patients, the severity of CAD was assessed in terms of the number of significantly stenosed coronary vessels (VD) and the Gensini score [18]. The coronary artery calcification (CAC) score was defined on CT images as the presence of more than two contiguous pixels with greater than 130 Hounsfield units. The CAC score in each lesion was then computed by the Agatston method [19].
Evaluation of risk factors for CAD
Body mass index (BMI), systolic blood pressure (SBP), diastolic BP (DBP), serum levels of TG, HDL-C, LDL-C, fasting blood glucose (FBG), hemoglobin A1c (HbA1c), smoking status, and medication use were collected as risk factors in all patients. BMI was calculated as weight (kg)/height (m)2. The characteristics of patients were obtained from medical records with regard to history of HTN, DL and DM.
Medications
Information on medication use was obtained from medical records and included biguanide, dipeptidyl peptidase-4 inhibitor (DPP-4I), insulin, angiotensin II receptor blocker/angiotensin-converting enzyme inhibitor (ARB/ACEI), calcium channel blocker (CCB), β-blocker and diuretics.
Statistical analysis
A statistical analysis was performed using Excel 2016 (SSRI, Tokyo, Japan) and the Stat View statistical software package (Stat View 5; SAS Institute Inc., Cary, NC, USA). Continuous variables are shown as the mean ± standard deviation. Categorical and continuous variables were analyzed for trends among the groups by the Cochran-Armitage trend test and Jonckheere-Terpstra trend test, respectively. A value of P < 0.05 was considered significant.Go to:
Results
Patient characteristics
One thousand sixteen patients were assessed for eligibility (Fig. 1). Three hundred fifty patients were excluded because they were receiving anti-lipidemic therapies. Six hundred sixty-six patients were divided into three groups: LDL-C < 70 mg/dL (n = 25, Low LDL-C group), 100 mg/dL > LDL-C ≥ 70 mg/dL (n = 141, Middle LDL-C group) and LDL-C ≥ 100 mg/dL (n = 500, High LDL-C group) (Table 1). The mean levels of LDL-C in the Low LDL-C, Middle LDL-C and High LDL-C groups were 57 mg/dL, 87 mg/dL and 133 mg/dL, respectively (P for trend < 0.001). In addition, the mean levels of TG in the Low LDL-C, Middle LDL-C and High LDL-C groups were 125 mg/dL, 132 mg/dL and 136 mg/dL, respectively (P for trend < 0.001). There were no significant differences in age, HDL-C, rate of HTN, HbA1c, FBS, SBP or medications (the rates of biguanide, DPP4-I, CCB, β-blocker and diuretics). On the other hand, there were significant differences in the rates of males, smoking, DL, DM, insulin and ARB/ACEI, and BMI and DBP.
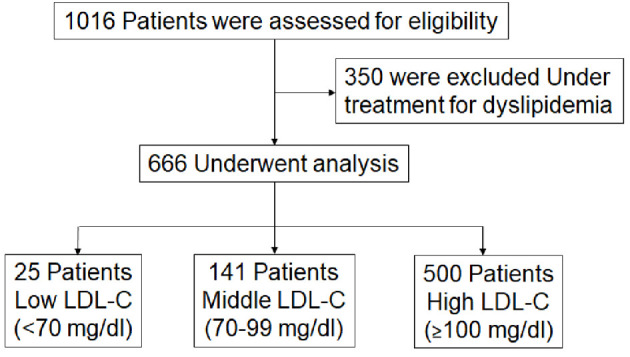
Flow chart of the enrollment process. LDL-C: low-density lipoprotein cholesterol.
Table 1
Patients Characteristics in All Patients, Low LDL-C, Middle LDL-C and High LDL-C groups
| All patients ( n = 666 ) | Low LDL-C ( n = 25 ) | Middle LDL-C ( n = 141 ) | High LDL-C ( n = 500 ) | P for trend | |
|---|---|---|---|---|---|
| (< 70 mg/dL) | (70 – 99 mg/dL) | (≥ 100 mg/dL) | |||
| Age (yrs) | 65 ± 13 | 64 ± 16 | 65 ± 13 | 65 ± 12 | 0.4 |
| Male, n (%) | 332 (50) | 15 (60) | 88 (62) | 231 (46) | < 0.001 |
| BMI, kg/m2 | 24 ± 4 | 23 ± 4 | 23 ± 3 | 24 ± 4 | 0.01 |
| Smoking, n (%) | 226 (34) | 10 (40) | 56 (40) | 160 (32) | 0.03 |
| DL, n (%) | 208 (31) | 6 (24) | 26 (18) | 176 (35) | < 0.001 |
| TG, mg/dL | 135 ± 100 | 125 ± 104 | 132 ± 145 | 136 ± 83 | < 0.001 |
| HDL-C, mg/dL | 57 ± 16 | 56 ± 24 | 56 ± 17 | 57 ± 16 | 0.3 |
| LDL-C, mg/dL | 120 ± 32 | 57 ± 13 | 87 ± 8 | 133 ± 26 | < 0.001 |
| DM, n (%) | 106 (16) | 1 (4.0) | 37 (26) | 68 (14) | 0.01 |
| HbA1c, % | 5.9 ± 0.8 | 5.7 ± 1.2 | 6.0 ± 1.0 | 5.9 ± 0.7 | 0.6 |
| FBS, mg/dL | 107 ± 27 | 104 ± 21 | 109 ± 27 | 106 ± 27 | 0.3 |
| HTN, n (%) | 386 (58) | 15 (60) | 86 (61) | 285 (57) | 0.2 |
| SBP, mm Hg | 135 ± 20 | 127 ± 20 | 134 ± 19 | 136 ± 20 | 0.1 |
| DBP, mm Hg | 78 ± 14 | 71 ± 15 | 77 ± 14 | 79 ± 13 | 0.02 |
| Medications | |||||
| Biguanide, n (%) | 31 (4.7) | 0 (0) | 8 (5.7) | 23 (4.6) | 0.5 |
| DPP4-I, n (%) | 49 (7.4) | 1 (4.0) | 15 (11) | 33 (6.6) | 0.1 |
| Insulin, n (%) | 10 (1.5) | 1 (4.0) | 6 (4.3) | 3 (0.6) | < 0.001 |
| ARB/ACEI, n (%) | 191 (29) | 7 (28) | 50 (36) | 134 (27) | 0.04 |
| CCB, n (%) | 210 (32) | 8 (32) | 51 (36) | 151 (30) | 0.1 |
| β-blocker, n (%) | 47 (7.1) | 2 (8.0) | 7 (5.0) | 38 (7.6) | 0.2 |
| Diuretics, n (%) | 55 (8.3) | 2 (8.0) | 11 (7.8) | 42 (8.4) | 0.4 |
The prevalence of CAD, number of VD, Gensini score and CAC score
When ≥ 50% of coronary stenosis was defined as significant stenosis, the prevalence of CAD values in the Low LDL-C, Middle LDL-C and High LDL-C groups were similar, at 52%, 47%, and 46%, respectively (P for trend 0.3) (Fig. 2a). The number of VD in the Low LDL-C, Middle LDL-C and High LDL-C groups was 0.8, 0.9 and 0.8, respectively (P for trend 1.0) (Fig. 2b). The Gensini score and CAC score were also similar between the groups (Fig. 2c, d). In addition, when ≥ 70% of coronary stenosis was defined as significant stenosis, there were also no differences in %CAD and the number of VD among Low, Middle and High LDL-C groups (Fig. 2e, f).
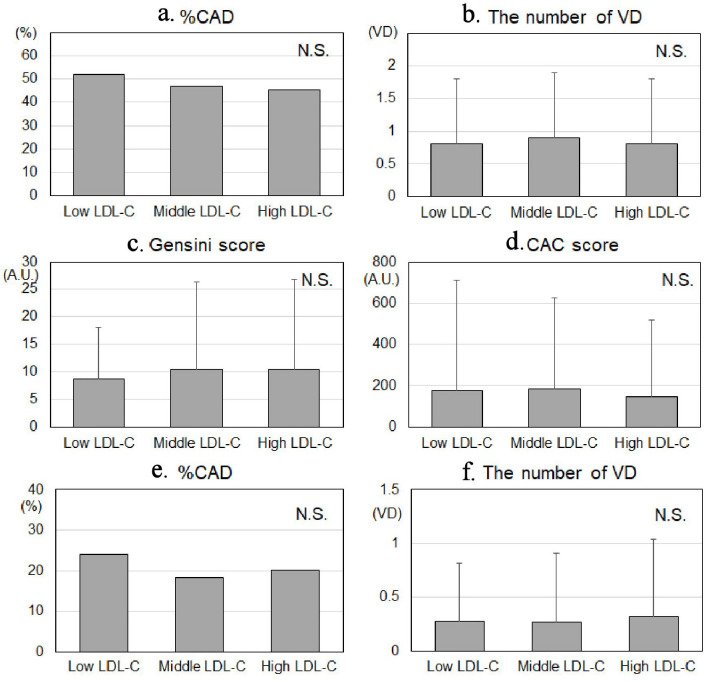
The prevalence of CAD (a, e), number of VD (b, f), Gensini score (c) and CAC score (d) in the Low LDL-C, Middle LDL-C and High LDL-C groups. The ≥ 50% and ≥ 70% of coronary stenosis were defined as significant stenosis in (a, b) and (e, f), respectively. CAD: coronary artery disease; number of VD: number of significantly stenosed coronary vessels; CACS: coronary artery calcium score; LDL-C: low-density lipoprotein cholesterol; N.S.: not significant; A.U.: arbitrary unit.
Author information
aDepartment of Cardiology, Fukuoka University Nishijin Hospital, Fukuoka, Japan
bDepartment of Cardiology, Fukuoka University School of Medicine, Fukuoka, Japan
cThese authors contributed equally to this manuscript.
dCorresponding Author: Shin-ichiro Miura, Department of Cardiology, Fukuoka University School of Medicine, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan.