Effects of Holding Beta-Blockers on the Vital Signs of Heart Failure Patients
Background
Heart failure with reduced ejection fraction (HFrEF) is associated with recurrent hospitalizations and high mortality. Guideline-directed medical therapy (GDMT) reduces morbidity, mortality and re-admission rates. Despite the evidence, less than 50% of patients with HFrEF are prescribed appropriate medical therapy. When hospitalized patients have these medications discontinued on admission or during hospitalization, they are less likely to have them restarted on discharge. The goal of this study was to determine the incidence of disruption of beta-blocker (BB) therapy during hospitalization for HFrEF patients admitted to an academic tertiary referral hospital.
Methods
We conducted a retrospective study in a single teaching hospital over the course of 1 year, and utilized data queried from the electronic medical record (EPIC) database. Inclusion criteria were met by patients with an ICD-10 code diagnosis of heart failure, left ventricular ejection fraction less than 40% and BB prescription prior to admission. Additional information noted included age, sex, vital signs throughout the admission and dates where BB was not given for a full 24-h period. Patients in the intensive care unit (ICU) were excluded due to uncertainty of their hemodynamics. Data were extracted from the electronic medical record database and analyzed through Python, Microsoft Excel and RStudio. The incidence of BB disruption during hospitalization was defined as a 24-h period where no BB was administered. Blood pressure (BP) and heart rate (HR) levels were compared between patients who received BB and patients who had a disruption in their BB. Measurements were also obtained to assess whether a correlation exists between holding BB therapy and time of the year, age, or sex.
Results
Between January 2018 and January 2019, 780 patient encounters met inclusion criteria for the study. Patients who were continued on BB therapy had an average BP of 120.8/68.7 mm Hg and an HR of 82.4 bpm on days they received their BB. Patients who had a disruption of BB therapy had an average BP of 117.7/67.6 mm Hg and an HR of 88.6 bpm on the days of the disruption (P < 0.001). There was no association between holding BB and age, sex, or time of year.
Conclusions
This study showed that in an academic tertiary referral center, patients with HFrEF who are not in an ICU have a 23% chance of not receiving their recommended BB therapy for 24 h. While the differences measured for BP and HR are statistically significant, they are not clinically significant.
Introduction
Heart failure is associated with high healthcare resource utilization, high mortality and high morbidity. Patients with an ejection fraction less than or equal to 40% have been shown to have reduced morbidity and mortality with the initiation of guideline-directed medical therapy (GDMT). Multiple seminal trials have shown mortality benefits of beta-blocker (BB) use in heart failure with reduced ejection fraction (HFrEF) patients, first with bisoprolol and metoprolol succinate in the CIBIS-II and MERIT-HF trials of 1999, respectively, later joined by carvedilol in the COPERNICUS trial of 2002 [1–3]. More recently, the BB-META-HF Study showed that BBs significantly reduce mortality in HFrEF patients with moderate to severe kidney dysfunction [4]. The ACCF/AHA Guidelines for the Management of Heart Failure include class I recommendations for the use of the aforementioned BBs in stage B and C HFrEF patients for the reduction of mortality, as well as the continuation of GDMT in hospitalized HFrEF patients. Furthermore, these guidelines promote the maximally tolerated doses of medication to achieve neurohormonal blockade [5, 6]. Despite the evidence showing the benefits of GDMT [1–3, 7, 8, 9–11], less than 20% of patients are prescribed optimal GDMT at appropriate doses [12].
In the inpatient setting, optimization of GDMT can be achieved with close monitoring in a controlled environment. This can be achieved by internists, hospitalists, family medicine physicians, or cardiologists. Obvious hurdles to optimization of GDMT in this setting are administrative pressures to reduce hospital duration and acute illness compromising the ability to up-titrate these medications appropriately [13]. Lack of nursing familiarity with HFrEF can result in holding these medications out of concern for precipitating iatrogenic cardiogenic shock. Despite previous studies showing minimal effects of BBs on blood pressure in heart failure patients, this represents a significant concern for nursing staff [12, 14, 15]. We sought to evaluate these concerns by investigating the differences in blood pressure on days where BBs were held versus days BBs were provided to patients with HFrEF.Go to:
Materials and Methods
Study design
This was a retrospective cohort study conducted at a single tertiary care center between January 2018 and January 2019. Our primary objectives were to determine the hold rate of BBs in patients with heart failure who had previously been on BBs and to determine the difference in vital signs between days BBs were given versus days BBs were held. A BB was considered held for that day if no BBs were administered in a 24-h period. If even one dose was given that day, it was considered a day in which the patient received therapy. Secondary objectives were to determine the length of hospital stay and to assess any differences in hold rates based on pharmacologic agent, age, month and gender. This study was approved by the Institutional Review Board at Erlanger. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Data collection
Data were collected from the electronic medical record (EMR) (EPIC) through secure data request. Patients were identified by an admission date between January 2018 and January 2019 along with a history of heart failure as identified by any associated ICD-10 code. The broad nature of this ICD-10 (I50) code necessitated a manual verification of patient status as “heart failure with reduced ejection fraction”. From this cohort, we acquired all vital signs during admission, the timing of the vital signs, age of the patient at time of admission, gender, type of BB prescribed and specific dates where BB therapy was held for 24 h. For BBs dosed more than once a day, all doses had to be missed to be considered a missed date.
Limitations
This model of data collection presents a new and novel way to rapidly collect data; however, it does lack specificity. The goal is to leverage large volumes of raw data to improve the signal-to-noise ratio in order to prove that further research would be fruitful. Our EMR does not mandate providing a rational why medications are held, therefore we only have the reported vitals proximal to the event. Different providers input their diagnoses to varying specificities, and these may not be recorded in a way that is explicitly searchable. This limits our ability to stratify patients based on co-morbidities. The history of HFrEF was investigated manually; however, the degree of severity was not reported in a universal way, such as with 5% increments estimated. While we know what medications were prescribed during the hospitalization, it is readily available which dosage was held on a given day. These limitations in specificity reduce our ability to establish a causal link. Future studies will be able to investigate these more specific questions. Future studies will also use more advanced post processing methods to rule out outlier data points.
Data analysis
Data were analyzed using a combination of software packages including Python (general data formatting) and RStudio (data analysis). Continuous variables were compared utilizing the Welch’s paired t-test. P values less than 0.05 were considered significant.Go to:
Results
Patient characteristics
Between January 2018 and January 2019, 780 patients (539 men and 241 women) were identified who met our inclusion criteria of being admitted to Erlanger main campus, with a total of 927 hospital admissions in that time span. Patients had a slightly higher mean systolic blood pressure on days where they received BB therapy compared to when they did not (120.5 mm Hg vs. 117.6 mm Hg, P < 0.001) (Fig. 1), a slightly higher diastolic blood (68.7 mm Hg vs. 67.6 mm Hg, P < 0.001) (Fig. 2) and a slower heart rate (82.4 bpm vs. 88.6 bpm, P < 0.001) (Fig. 3) (Table 1). The mean duration of stay for patients on carvedilol and metoprolol was 7.02 and 8.8 days, respectively (P < 0.05) (Fig. 4). There was no difference associated with age or gender (Figs. 5 and 6). The average hold rate of BBs for any given day in a year was 23% (Fig. 7).
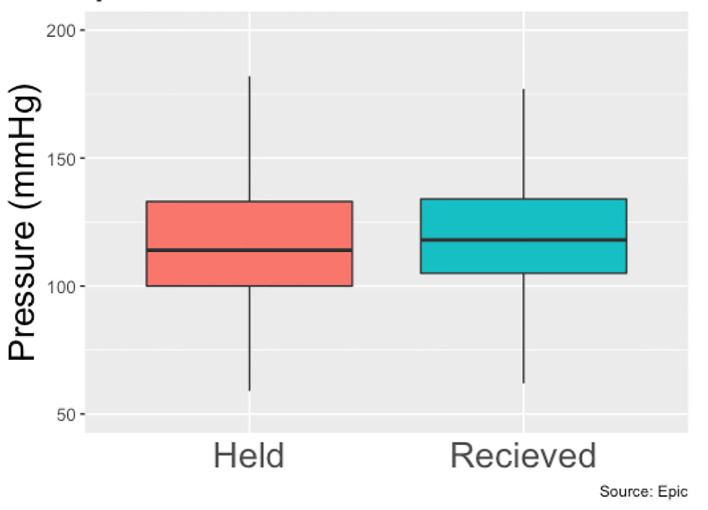
Systolic pressures of patients with held beta-blockers vs. received beta-blockers.
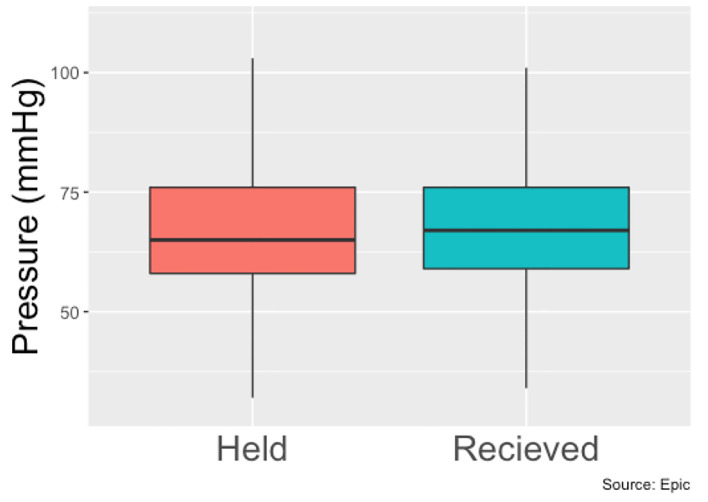
Diastolic pressure of patients with held beta-blockers vs. received beta-blockers.
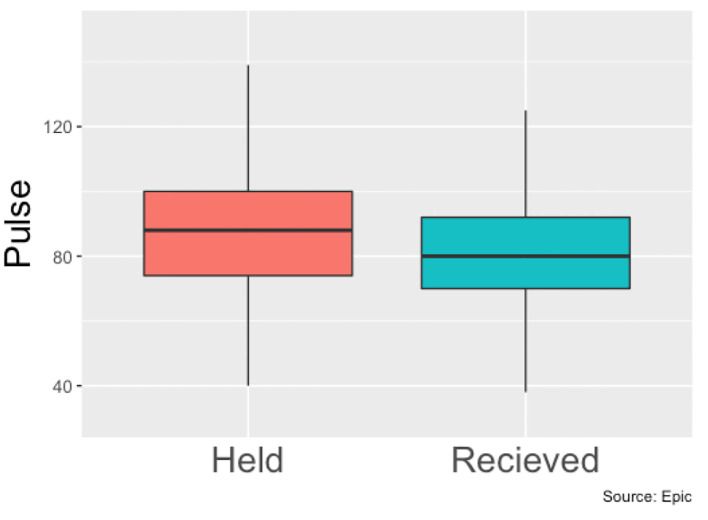
Heart rates means of patients with held beta-blockers vs. received beta-blockers throughout hospital stay.
Table 1
Hemodynamic Data Among Patients With Held and Received Beta-Blockers
| Received | Held | Difference | P value | |
|---|---|---|---|---|
| Systolic BP | 120.8 | 117.7 | -3.1 | < 0.001 |
| Diastolic BP | 68.7 | 67.6 | -1.1 | < 0.001 |
| Heart rate | 82.4 | 88.6 | 6.2 | < 0.001 |
BP: blood pressure.
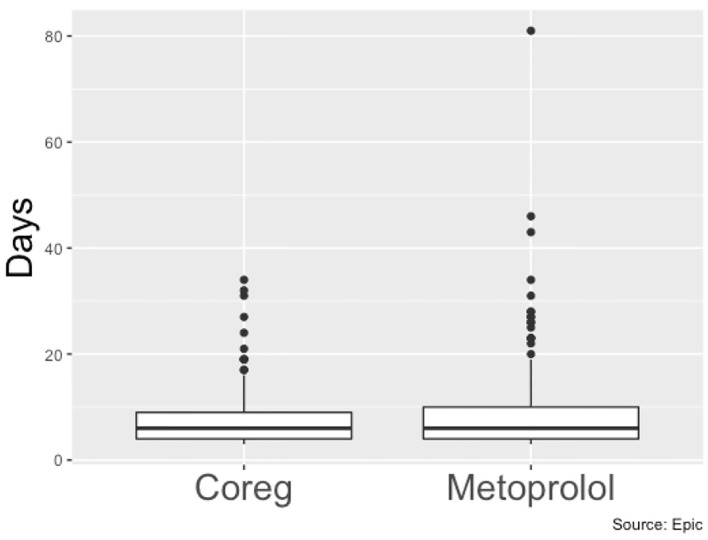
Length of stay (days) of patients on carvedilol vs. patients on metoprolol.
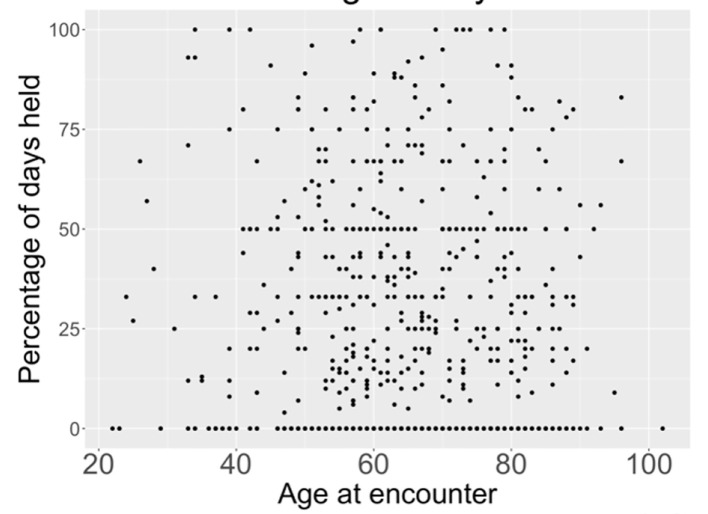
Relationship between age and percentage of days held.
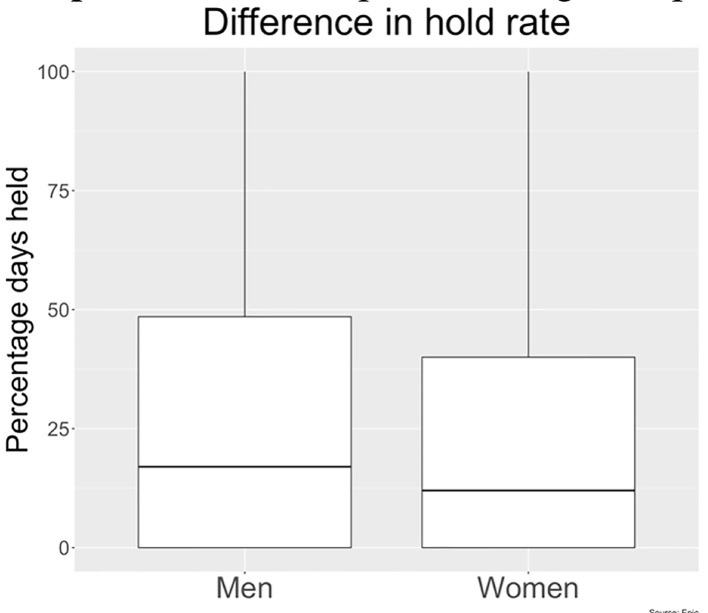
Beta-blocker hold rate in men vs. women as observed in our study.
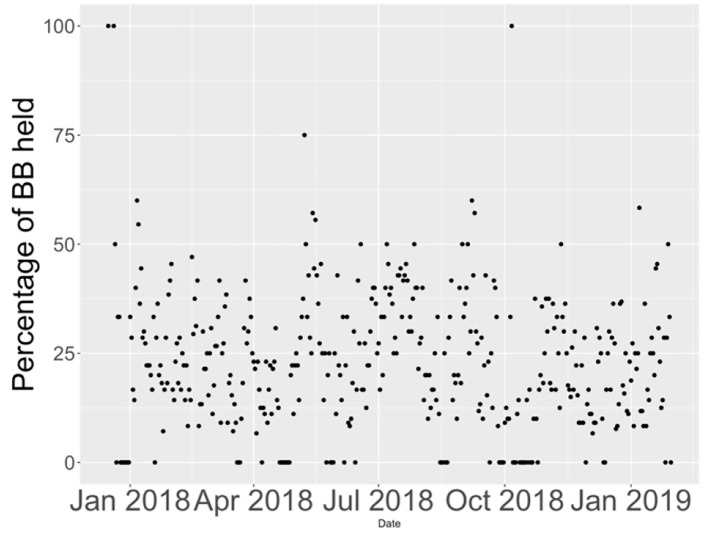
Percentage of beta-blockers held on floors from January 2018 to January 2019.
The data indicate that there is no clinically significant difference in the blood pressures of these patients on a day-to-day basis. These findings are consistent with previous findings that cardiac remodeling occurs over the span of months. This information confirms clinical intuition that BBs should not be held purely on blood pressure as there is no meaningful difference in blood pressure on the days the BBs were held. BBs should only be held for symptoms. Changes in blood pressure throughout the day were more consistent with diurnal rhythms than a consistent effect of medication (Fig. 8).
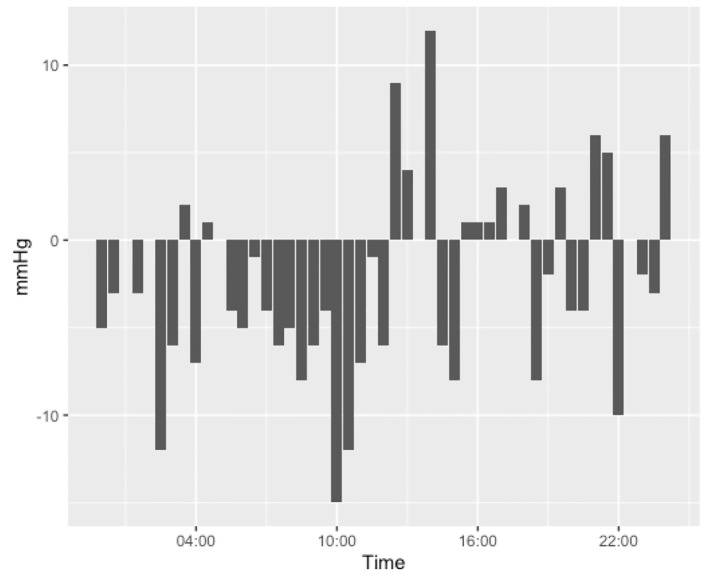
Difference in systolic pressures between patients who had their beta-blockers held against those who received their beta-blocker, divided into 30-min increments throughout the day. Figure was created from data from EPIC.
Author information
aDepartment of Cardiology, University of Tennessee at Chattanooga, 975 E 3rd Street, Chattanooga, TN 37403, USA
bCorresponding Author: Marc Erickson, Department of Cardiology, University of Tennessee at Chattanooga, 975 E 3rd Street, Chattanooga, TN 37403, USA.