Extensive Frontoparietal Abscess: Complication of Frontal Sinusitis (Pott’s Puffy Tumor)
Raquel Andrade Lauria,* Fernando Laffitte Fernandes, Thiago Pires Brito, Pablo Soares Gomes Pereira, and Carlos Takahiro Chone
Case Report
A 14-year-old male adolescent, with no significant past medical history, presented at an otorhinolaryngology department of a tertiary teaching hospital with a 7-day history of a common cold that progressively evolved with frontal headache, vomiting, fever, purulent rhinorrhea, and frontal and periorbital swelling. He had been treated in another service where he remained hospitalized for eight days, being started on amoxicillin-clavulanate 3 g/day for seven days with partial improvement of periorbital edema. He maintained, however, daily fever and progressive worsening of the frontal swelling.
Physical examination on admission revealed extensive painful and fluctuant swelling of the forehead and parietal region, periorbital edema, and spontaneous purulent lacrimal discharge (Figure 1a). Anterior rhinoscopy showed a hyperemic mucosa, nonobstructive turbinates, and mucopurulent discharge in common meatus bilaterally. Nasofibroscopy showed bilateral frontal recess purulent discharge, greater on the left. It showed no neurological abnormalities or signs of systemic involvement. The remainder of the physical exam was unremarkable.
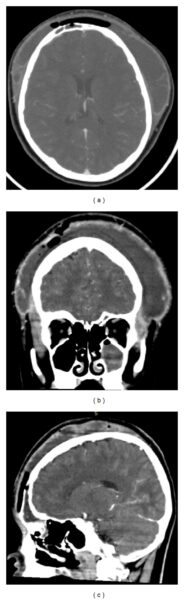
Figure 1
Axial (a), coronal (b), and sagittal (c) CT without contrast demonstrating soft tissue swelling of the forehead and parietal region; erosion of anterior table of the frontal sinus; frontal, maxillary, and anterior ethmoid sinuses opacification; subcutaneous emphysema.
Patient underwent CT scan of the paranasal sinuses which showed the following changes: erosion of anterior table of the frontal sinus, frontal, maxillary, and anterior ethmoid sinuses opacification, subcutaneous emphysema, and soft tissue swelling of the forehead and parietal region.
Due to the abscess extension, the patient was opted for surgical drainage with combined approach (endoscopic endonasal and external drainage via coronal incision), with drainage of approximately five hundred milliliters of thick purulent fluid sent for culture (Figure 3(a)). Intraoperative inspection showed frontal and temporal muscles necrosis, associated with osteomyelitis and erosion of the external table of the frontal bone. Additionally, endoscopic intranasal frontal sinusotomy was performed. (Figures 3(b), 3(c), and 3(d)).

Figure 3
Intraoperative images. Thick purulent secretion (a). Erosion of the outer table of the frontal bone, necrosis of the temporal muscle and frontal sinus combined approach surgery (b). Penroses drains placed (c). Final appearance after suture of bicoronal incision (d).
The patient was admitted to the intensive care unit and recovered well postoperatively, afebrile, and with remission of complaints. Culture grew Streptococcus constellatus susceptible to multiple antibiotics. He was prescribed intravenous antibiotic therapy throughout hospitalization, treated with metronidazole 2 g/day for five days associated with vancomycin 2 g/day and ceftazidime 6 g/day maintained for 18 days. The combination of antibiotics was initially chosen guided by common microorganisms associated with this entity and adjusted according to results of antibiogram, with suspension of metronidazole. Due to suspicion of adverse drug reactions, the antibiotics were exchanged for ampicillin-sulbactam, maintained for seven more days. He was discharged on the 25th postoperative day asymptomatic and with normal physical examination, showing no new complaints in the follow-up so far (Figure 2(b)).
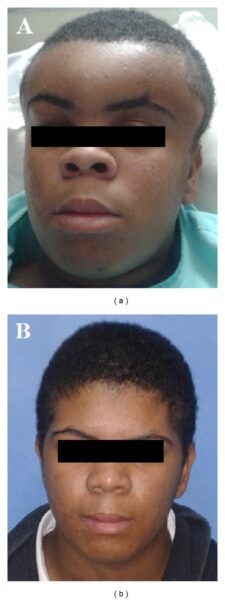
Figure 2
Preoperative image of the patient showing extensive forehead swelling (a), 40th postoperative day (b).
References
Ketenci I, Ünlü Y, Tucer B, Vural A. The Pott’s puffy tumor: a dangerous sign for intracranial complications. European Archives of Oto-Rhino-Laryngology. 2011;268(12):1755–1763. [PubMed] [Google Scholar]
Suwan PT, Mogal S, Chaudhary S. Pott’s Puffy tumor: an uncommon clinical entity. Case Reports in Pediatrics. 2012;2012:4 pages.386104 [PMC free article] [PubMed] [Google Scholar]
Haider HR, Mayatepek E, Schaper J, Vogel M. Pott’s puffy tumor: a forgotten differential diagnosis of frontal swelling of the forehead. Journal of Pediatric Surgery. 2012;47:1919–1921. [PubMed] [Google Scholar]
Kim H, Hwang EH, Han YM, Kim SH, Kim YM. Pott’s puffy tumor in an adolescent boy. Pediatrics International. 2012;54:158–160. [PubMed] [Google Scholar]
Jung J, Lee HC, Park I, Lee HM. Endoscopic endonasal treatment of a Pott’s puffy tumor. Clinical and Experimental Otorhinolaryngology. 2012;5:112–115. [PMC free article] [PubMed] [Google Scholar]
Parida PK, Surianarayanan G, Ganeshan S, Saxena SK. Pott’s puffy tumor in pediatric age group: a retrospective study. International Journal of Pediatric Otorhinolaryngology. 2012;76:1274–1277. [PubMed] [Google Scholar]