Facial Tissue Allotransplantation
Case Report
Patient E, a 19-year-old man, was admitted to hospital for treatment of third- to fourth-degree electrical burns to 17% of the surface of the head, neck, and right upper and lower limbs. He was injured on August 09, 2012, in the line of duty while performing military service. Over the period of 3 years, he received >30 reconstructive surgeries, which were performed with the aim of closing the defects, as well as to restore vision, and regain functioning of the affected limbs. However, the results of treatment were not sufficient to allow the patient to achieve social adaptation and did not eliminate the major self-identification disorder which he developed after the facial injury. This caused him to attempt suicide on 2 occasions. All possibilities for plastic reconstructive surgery were exhausted, and in view of deficiency of the covering tissues, it was decided to perform allotransplantation of a complex face tissue allograft for patient E.
It is important to note that after the traditional surgical treatment, functional disorders of the damaged right half of the face were insignificant. The main and most difficult target of the reconstruction was the central zone of the face (Fig.1).

Appearance of patient E, after the completion of traditional rehabilitation treatment and before facial allotransplantation.
During preparation of the potential recipient for face allotransplantation, informed consent was obtained for the surgery. The patient was fully examined according to the international pretransplantation protocol.
For the purposes of detailed assessment of the damage, the patient underwent several series of 3-dimensional (3D) laser scans of the face, followed by printing out the areas of defect using a 3D printer. This allowed us to carry out more accurate modeling and anatomical positioning of the allograft, both during preparation for the surgery and during the procedure itself (Figs. 2 and 3).
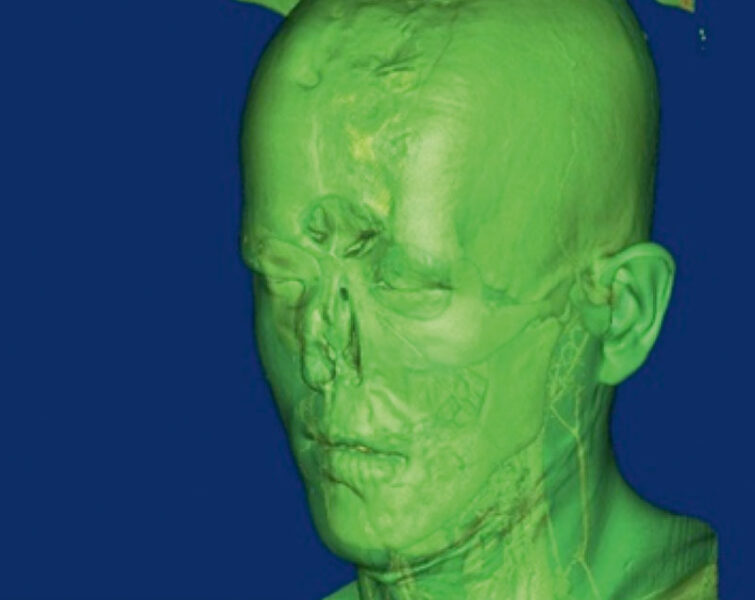
Scan of the patient’s face during the preparations for allotransplantation surgery.
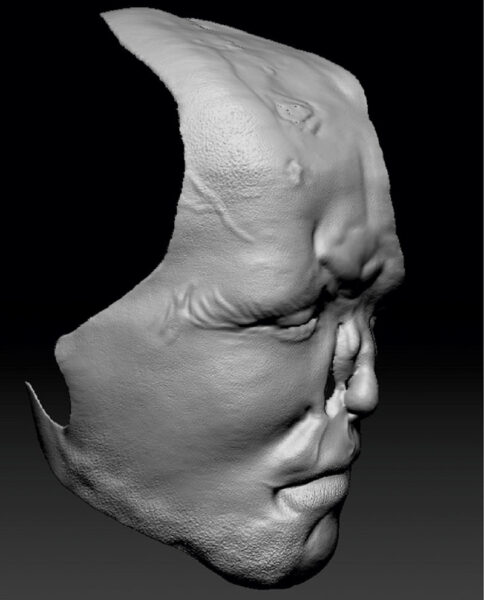
Three-dimensional print of the surface of patient E’s facial deformity.
Donor Stage
In May 2015, the Coordination Center received information about a potential male donor of 51 years of age with a traumatic brain injury and started the procedure for ascertaining brain death. Laboratory, instrumental and immunological studies determined compatibility with the recipient.
After the pronouncement of brain death, intensive therapy of the donor continued, aimed at prevention of purulent-septic complications, correction of water and electrolyte balance, hypotension, hyperglycemia, polyuria, and hypothermia. Consent was obtained from the relatives of the deceased to explant facial tissues.
The facial allotransplantation algorithm was divided into 3 consecutive stages, with repeated training in the operating theater using cadaveric material.
Stage 1. Explantation of the Facial Tissue Complex and Closure of the Defect with a Death Mask
The allograft explantation was performed according to the “full-face” model, with involvement of the facial artery and vein. After complete dissection of the facial allograft, the mucous membrane of the ethmoid sinus and external wall of the frontal sinuses were removed, and the external carotid artery was cannulated, followed by conservation with Custodiol HTK Solution (Essential Pharmaceuticals, LLC) cooled to 2°C. Perfusion efficiency was determined by the change in the color of the graft and the outflow of the solution through the venous system. Duration of the explantation was 7 hours 15 minutes.
According to the principles of humane treatment of the body of a deceased person, the donor’s facial tissue defect was closed with a death mask (Fig. 4). At the final stage of manufacturing the death mask, the finished silicone model of the face was cleaned of artifacts, eyebrows and eyelashes were fixed, and makeup was applied. Preparation of the mask took about 8 hours.

Manufacturing stages of the donor’s death mask.
Stage 2. Preparation of the Recipient
Preparation of the recipient bed consisted of removing granulating tissues from the cavity of the frontal sinuses, excision of affected tissues in the upper and middle zone of the face within the defect area, and isolation of the external jugular vein and external carotid artery on the right and on the left.
Stage 3. Allotransplantation of the Facial Tissue Complex
This surgical stage included the following tasks: modeling, inclusion of the allograft into the bloodstream, and adaptation of its bone and soft-tissue complex of tissues in the donor-recipient system.
Inclusion of the allograft into the bloodstream was by means of end-to-side anastomosis of the recipient’s external carotid artery with the donor’s facial artery on the right, and of the recipient’s external jugular vein with the donor’s facial vein on the left. Standard methods were used to check the competence of the anastomoses and to obtain a sufficient capillary response from donor tissues, including at distal level (Figs. 5 and 6).

Integration stage of the donor’s allograft to cover the facial deformity of the recipient.

Microsurgical stage showing arterial and venous anastomoses.
The osteoplastic stage included tamponade of the frontal sinuses with a free-muscle autograft (Fig. 7), anatomical positioning of bone and soft-tissue structures of the allograft, and their fixation to the recipient bed with miniplates (Figs. 8-9).

Tamponade of the patient’s frontal sinus with the tissues of the patient’s own free muscle flap of the thigh.

Appearance of patient E at the final stage of the facial allotransplantation operation.
During the surgery, the recipient underwent allotransplantation of a “signal” Chinese flap in the lower third of the left forearm, to obtain biological material for step-by-step biopsies for histological and immunohistochemical studies throughout the lifetime of the donor tissues (Fig. 9).

Appearance of the forearm of patient E after the transplantation of Chinese flap.
Immunological Protocol
The immunosuppressive therapy protocol was divided into initial and supporting stages. In accordance with the adopted protocol, a control biopsy of the skin signal flap was performed on days 3, 7, 14, 21, and 30, and every month after that (Fig. 10).

Appearance of patient E 2 years post partial facial allotransplantation operation.
The following complications were observed after the face allotransplantation: disseminated intravascular coagulation syndrome, acute respiratory distress syndrome, moderate posthemorrhagic iron-deficiency anemia, moderate thrombocytopenia, systemic inflammatory reaction syndrome, and false aneurysm of the facial artery on the right. Standard infusion-transfusion, respiratory, and antibacterial therapy was administered, supplemented with hemodiafiltration as needed.
The most stressful complication was thrombosis of the donor vein that occurred during the first day after the surgery.
Condition of the Patient at the Present Time
One year after the partial face allotrasplantation, the patient underwent rhinoplasty aimed at reduction of the volume of tissues at the end part of the nose and restoration of the columella (Fig. 11 ).

Appearance of patient E. 3 years post partial facial allotransplantation operation.
Complete social rehabilitation of the patient has now been achieved. He attends an institution, works, and has a family.
Author information
From the *State Budget Institution of Higher Education, North-Western State Medical University named after I.I. Mechnikov, Ministry of Public Health of the Russian Federation, Saint Petersburg, Russian Federation†State Budget Institution of Higher Education, Military Medical Academy named after S.M. Kirova, Saint Petersburg, Russian Federation‡State Budget Institution of Higher Education, Russian National Research Medical University named after N.I. Pirogov, Ministry of Public Health of the Russian Federation, Moscow, Russian Federation§The Federal Medical-Biological Agency, Moscow, Russian Federation.Corresponding author.
Maria Volokh, Kirochnaya ul. 41, 191015, Saint-Petersburg, Russian Federation
Copyright
Copyright © 2019 The Authors. Published by Wolters Kluwer Health, Inc. on behalf of The American Society of Plastic Surgeons.