Reconstruction of a Missing Midface
An 18-year-old Chinese girl was referred to us with a severe facial deformity that had been present since her birth. The deformity was associated with poor speech intelligibility and feeding disturbances. Clinical examination demonstrated a severe maxillary defect and bilateral zygoma hypoplasia accompanied by nose and mandible deformities. Her mouth opening was normal, and no obvious deviation of the mandible was observed. No teeth presented in her upper jaw, and the teeth in the lower jaw were intact but lingually inclined. A three-dimensional computed tomography scan clearly revealed the patient’s skeletal deformity (Fig. 1). The patient’s health and social life were greatly affected, and she had a high motivation to undertake any procedure that would improve her oral–facial function and appearance. In addition, the patient’s family history could not be traced because she had been abandoned as a baby.

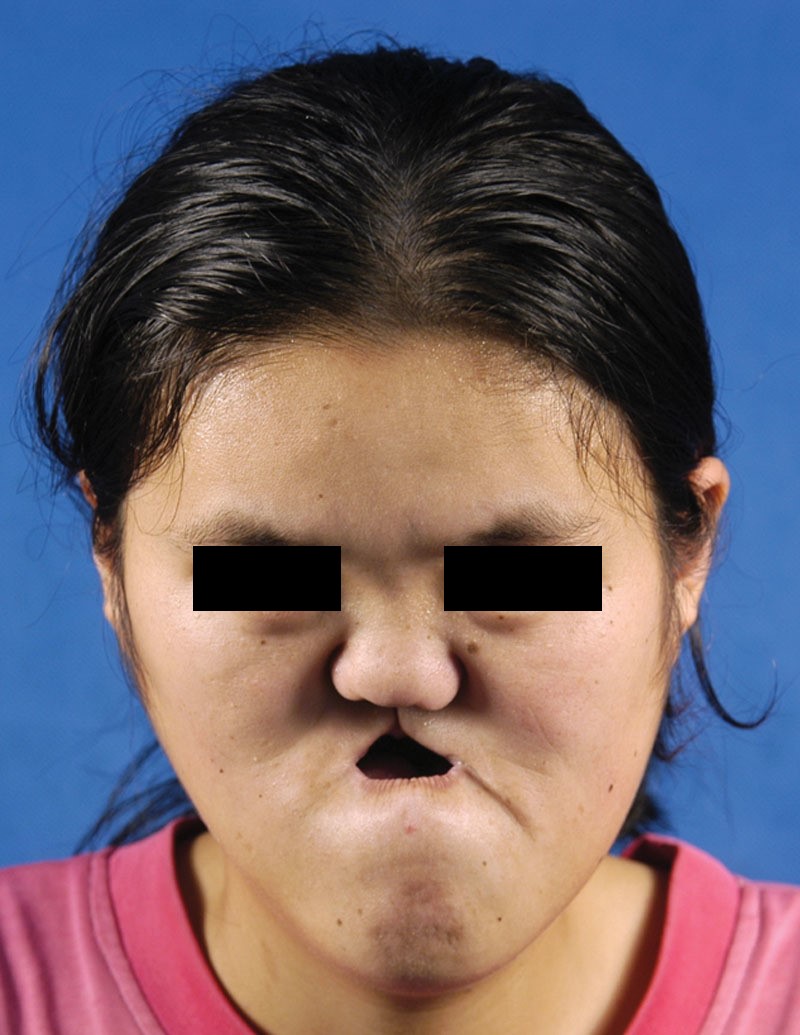
The front view of the patient showed an obvious facial deformity with serious hollow midface and deviated lower jaw.
They adopted a comprehensive strategy to reconstruct a new midface for the patient. After an extensive multidisciplinary discussion among the maxillofacial surgeons, orthodontists, and prosthetic teams, we began the treatment with the correction of her hypoplastic zygoma and nasal bone by performing a Le Fort III osteotomy and external DO. The distraction distance was 1.6 cm, and the girl acquired a fronted zygoma and nasal bone, and her orbital shape was also improved greatly (Fig. 2).
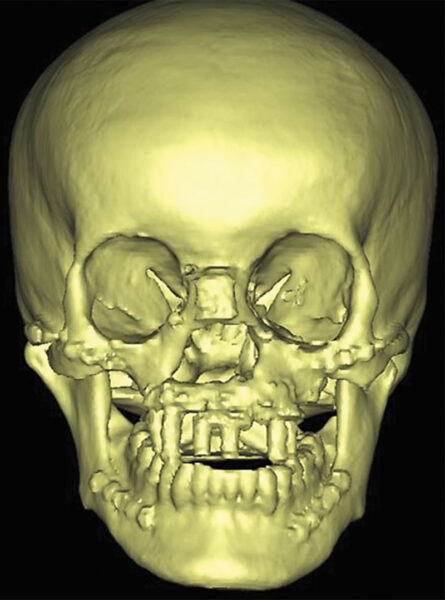
The three-dimensional computed tomography demonstrated that the maxilla was almost completely missing, the mandible was obviously asymmetry, and the zygomas were bilaterally hypoplasia as well.
Because of the severe deficiency in the midface, we decided to use a fibula osteomyocutaneous flap to rebuild a new maxilla. We manufactured resin models of a facial skeleton and a fibula bone according to computed tomography data and performed model surgery. The miniplates were prebent to facilitate shaping the fibula graft and to ensure its proper placement during surgery. Then, a 19.5-cm long fibular bone with a 3 × 8-cm2 skin paddle was harvested and shaped to form a U-shaped maxillary arch that was connected to the bilateral zygoma and the remnant thin maxilla (Fig. 2). The skin island and muscle were placed into the mouth to separate the nasal and oral cavities. After surgery, the patient’s facial contour was dramatically improved.
To rebuild an appropriate occlusion and further improve the facial contour, we performed implantation in the reconstructed maxilla and mandible osteotomy (bilateral sagittal split ramus osteotomy). We designed and produced an implant guide and a special splint, which was composed of the implant guide and a mandible occlusal guide, using the computer-aided design/computer-aided manufacturing technique. Five implants were placed, and the mandible was moved backward (Fig. 3). Three months later, vestibuloplasty was performed, and the rhinoplasty was then conducted with a costal cartilage graft to improve the patient’s nasal profile. The final dental prosthesis was attached with implants.
After reconstructive surgery was completed, the patient acquired a new maxilla formed by fibula and the augmented zygomas. Then 5 implants were inserted into the fibula bone, and bilateral sagittal split ramus osteotomy surgery was completed under the conduction of digitally designed splint.
It took 3½ years to complete the entire treatment process. The patient recovered very well, and no obvious complications were referred to us (Fig. 4). She married and gave birth to a healthy boy during the follow-up period.

The front and lateral view of the patient after the final dental prosthesis was fitted.
Author information
From the *Department of Cranio-facial Trauma and Orthognathic Surgery, College of Stomatology,
†The Key State Laboratory of Military Stomatology, and ‡Department of Prosthodontics, College of Stomatology, Fourth Military Medical University, Xi’an, China.
Corresponding author.Yimin Zhao, PhD, DDS, Department of Prosthodontics, School of Stomatology, Fourth Military Medical University, 145 West Changle Road, Xi’an 710032, China