Reconstructive Knee Surgery
Shin-Taeg Kang, Chan-Ha Hwang,Bo-Hyeon Kim, and Byung-Yoon Sung*
CASE REPORT
Paramedics brought a 45-yr-old man into our medical center immediately after a high-velocity crush injury. On admission to the emergency room, the patient was noted to have a large open wound in anterior aspect of left knee. His left foot was pale and cool. Distal pulses of dorsalis pedis artery and posterior tibial artery were absent, and only femoral pulse was palpable on the injured left lower extremity. He was alert with respiratory rate of 22, pulse rate of 98, and blood pressure of 100/80. Neurological examination relating to his left leg was grossly normal.
The knee joint was open, and a portion of the patellar tendon was lost. About 50% of the patellar tendon was remained, but it was detached from the inferior pole of the fractured patella. Distal femoral condyle, and metaphysis were absent. All of the collateral ligaments and the cruciate ligaments of the knee were lost together. Only the biceps tendon and a portion of the semimembranosus tendon were attached to the proximal tibia and fibula around the knee. Plain radiography showed severe bone loss of distal femur, fractures of patella and proximal tibia (Fig. 1A). Femoral arteriography demonstrated a complete occlusion of the left popliteal artery (Fig. 1B).

(A) AP radiograph shows the severe comminuted fractures of the femur, tibia and patella, and severe loss of distal femoral bone. (B) Angiography demonstrates the complete occlusion of popliteal artery near to plateau of the tibia.
Our surgical orthopedic team performed an emergency operation within 4 hr of triage. First, we debrided contaminated soft tissue aggressively and fixed the patellar fracture. Then we repaired the ruptured patellar tendon with pull-out sutures through the patella. Primary fracture fixation of the distal femur was impossible because expelled fragments of the distal femur were lost. Prior to repair of the popliteal artery, we applied an external fixator across the knee joint. Then we positioned the patient in prone position to explore the popliteal artery. The same orthopedic surgical team explored the popliteal artery via posterior approach of knee. The left popliteal artery was contused but its continuity was maintained by adventitial tissue. We made a small longitudinal incision to a suspected portion of injury of the popliteal artery. The intima of the popliteal artery was torn and dissected, and a large thrombus occluded the popliteal artery completely (5). The popliteal vein was moderately contused, but tibial nerve was grossly intact. We excised a segment of the contused and thrombosed popliteal artery in 1.5 cm length. We were able to easily perform an end-to-end repair of the artery only with mild mobilization of the proximal part of the popliteal artery because severe bone loss of the distal femur made approximation of ends of the popliteal artery to be ease. After the direct repair of the popliteal artery, distal pulse was palpable and limb circulation was recovered. Then we waited for 30 min watching for circulation, swelling of the leg and compartment syndrome. We decided not to perform a fasciotomy of the low leg to prevent compartment syndrome because we could not find cyanosis, swelling or hardness of muscle compartments of the low leg, such as associated signs of compartment syndrome.
At 4 days after the emergency operation, we performed debridement again and inserted antibiotics (vancomycin)-mixed cement beads into the defect of the distal femur to prevent infection. The patient received 2nd-generation cephalosporin and aminoglycoside antibiotics during the initial 2 weeks and he received more 2nd-generation cephalosporin antibiotics during the following 2 weeks (Fig. 2).
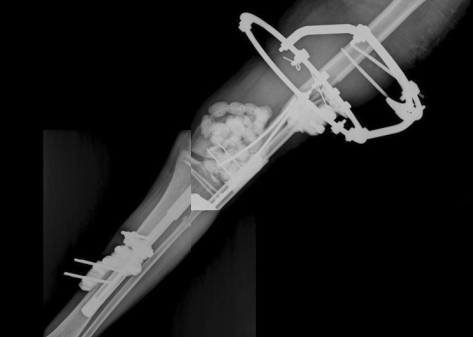
External fixator crossing the knee joint was applied and antibiotics-mixed cement beads were inserted into the defect of the distal femur.
After 6 weeks, we performed a reconstructive total knee arthroplasty with modular segmental endoprosthesis, MUTARS® (Implantcast, Buxtehude, Germany) to treat the large bone loss of the distal femur (Fig. 3). Simultaneously, we carried out patellar tendon augmentation using a semitendinosus allograft because gracilis and semitendinosus were lost at the initial trauma (Fig. 4A). Furthermore, a medial gastrocnemius rotational flap with meshed skin graft was followed because conditions of the repaired patellar tendon and anterior skin of the knee were not healthy for rehabilitation of the knee joint (Fig. 4B).
One week after the reconstruction, physiotherapy team commenced continuous passive motion of the knee and crutch ambulation began 2 weeks after reconstruction.
At his most recent follow-up visit, 36 months postoperatively, the patient does not complain of pain, and can ambulate without support. The range of motion of the knee joint is 10 degrees to 55 degrees. Power of quadriceps muscle is 4/5, and the knee society knee score in pain is 79 and functional score is 50. The patient shows a mild limping gait because of 1.5 cm shortening of the left leg after the reconstruction arthroplasty. However, the patient can ambulate independently and is satisfied with the results (Fig. 5).
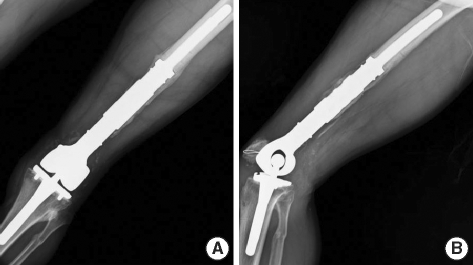
(A) Postoperative AP and (B) lateral radiographs at 36 months after reconstructive arthroplasty shows good alignment of the components and extracortical bone bridging.
Author information
Department of Orthopedic Surgery, Cheongju St. Mary’s Hospital, Cheongju, Korea.
*Department of Orthopedic Surgery, St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea.
corresponding authorCorresponding author.
Address for correspondence: Chan-Ha Hwang, M.D. Department of Orthopedic Surgery, Cheongju St. Mary’s Hospital, 589-5 Jujung-dong, Sangdang-gu, Cheongju 360-568, Korea.
Copyright and License information
Copyright © 2009 The Korean Academy of Medical SciencesThis is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
References
- Friedman SA, Cerruti MM, Kosmoski J, Sobel J. Isolated popliteal artery rupture caused by blunt trauma. Angiology. 1971;22:533–537. [PubMed] [Google Scholar]
- Lange RH. Limb reconstruction versus amputation decision making in massive lower extremity trauma. Clin Orthop Relat Res. 1989;243:92–99. [PubMed] [Google Scholar]
- Harrison RJ, Jr, Thacker MM, Pitcher JD, Temple HT, Scully SP. Distal femur replacement is useful in complex total knee arthroplasty revisions. Clin Orthop Relat Res. 2006;446:113–120. [PubMed] [Google Scholar]
- Springer BD, Sim FH, Hanssen AD, Lewallen DG. The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res. 2004;421:181–187. [PubMed] [Google Scholar]
- Eger M, Huler T, Hirsch M. Popliteal artery occlusion associated with dislocation of the knee-joint. Report of a case with successful surgical repair. Br J Surg. 1970;57:315–317. [PubMed] [Google Scholar]
- Tominaga GT, Connolly JE, Wilson SE. Bilateral popliteal artery injury from bumper crush injury. J Trauma. 1996;40:311–313. [PubMed] [Google Scholar]
- Frink SJ, Rutledge J, Lewis VO, Lin PP, Yasko AW. Favorable long-term results of prosthetic arthroplasty of the knee for distal femur neoplasms. Clin Orthop Relat Res. 2005;438:65–70. [PubMed] [Google Scholar]
- Dennis DA. The structural allograft composite in revision total knee arthroplasty. J Arthroplasty. 2002;17(4 Suppl 1):90–93. [PubMed] [Google Scholar]
- Petrou G, Petrou H, Tilkeridis C, Stavrakis T, Kapetsis T, Kremmidas N, Gavras M. Medium-term results with a primary cemented rotatinghinge total knee replacement. A 7-to 15-year follow-up. J Bone Joint Surg Br. 2004;86:813–817. [PubMed] [Google Scholar]
Articles from Journal of Korean Medical Science are provided here courtesy of Korean Academy of Medical Sciences

