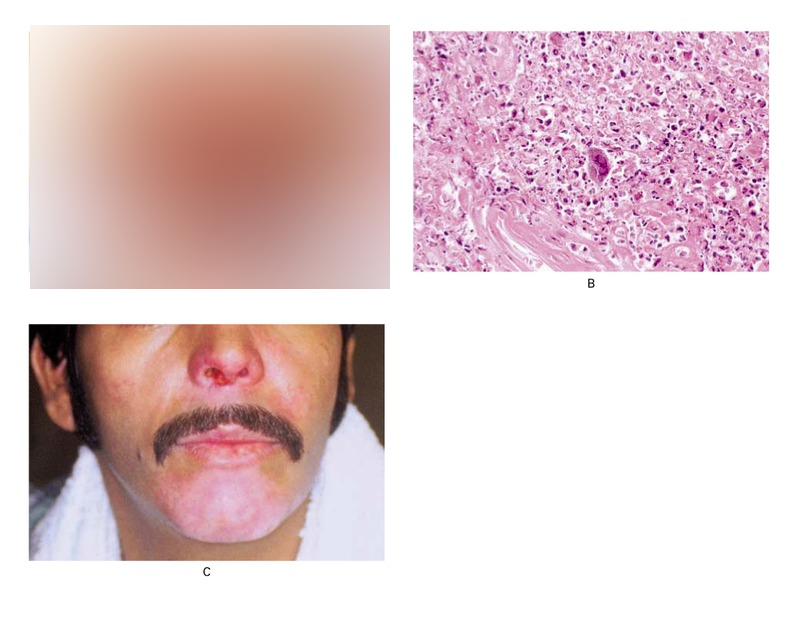
Severe Herpes Simplex infection on an HIV Patient
Figure 1 A 30-year-old man with the acquired immunodeficiency syndrome (CD4 cell count, 14 per cubic millimeter) presented with a six-month history of enlarging facial lesions. The lesions had not responded to a six-week course of oral acyclovir (800 mg five times a day). The patient had no history of herpes or any other opportunistic infections. His only other medications were dapsone and fluconazole. On examination, he was afebrile and had extensive, friable, hemorrhagic crusts with impetiginization of the chin and around the nares (Panel A). He also had aphthous ulcers on the soft palate and the anterior portion of the hard palate. The rest of the examination was unremarkable. A skin biopsy showed an acute inflammatory infiltrate and multinucleated giant cells with typical ground-glass nuclei (Panel B; hematoxylin and eosin, ×200), consistent with the presence of a herpetic infection; viral cultures of scrapings from the base of the lesion subsequently yielded herpes simplex virus. There was little improvement in the lesions after 10 days of intravenous therapy with acyclovir but complete resolution after intravenous foscarnet therapy (Panel C). The aphthous ulcers also improved. Treatment also included normal saline “wet-to-dry” dressings to soften and remove the crusts and mupirocin ointment.