Silicone Migration and Late Hematoma following Silicone Implant Rupture: Case Report and Literature Review
CASE REPORT
A 65-year-old woman with a history of bilateral silicone breast augmentation in 1987 and hypertension presented to clinic with swelling and discomfort of her inferior left breast (Fig. 1). She stated that the symptoms began after a motor vehicle collision 3 years prior. Since that time, the left breast implant had slowly developed significant swelling inferiorly, along with pain and tenderness of the overlying skin. She had initially presented to an outside institution for management, but, due to insurance reasons, could not obtain definitive management. She then presented to our institution nearly 3 years after the initial traumatic injury, during which time she remained hemodynamically stable and asymptomatic with regard to anemia.
Physical examination of the breasts revealed significant capsular contractures bilaterally along with a large, firm, immobile soft-tissue mass of the inferior left breast with overlying skin hyperemia and hypervascularity. In the right breast, there was extensive soft-tissue fullness along superior pole with extension into the axilla. A fluctuant, nontender, 8 × 4 cm soft-tissue mass was palpated within the right upper arm, overlying the medial aspect of brachialis muscle. No accompanying skin changes were seen over the mass. The patient denied systemic (type B) symptoms, skin breakdown, nipple discharge, or retraction, palliating the initial concern for cancerous neoplasm. Her last mammogram was approximately 3 years before presentation and showed no signs of malignancy. She had no prior history of breast cancer. She denied taking any medication with anticoagulant or antiplatelet activity.
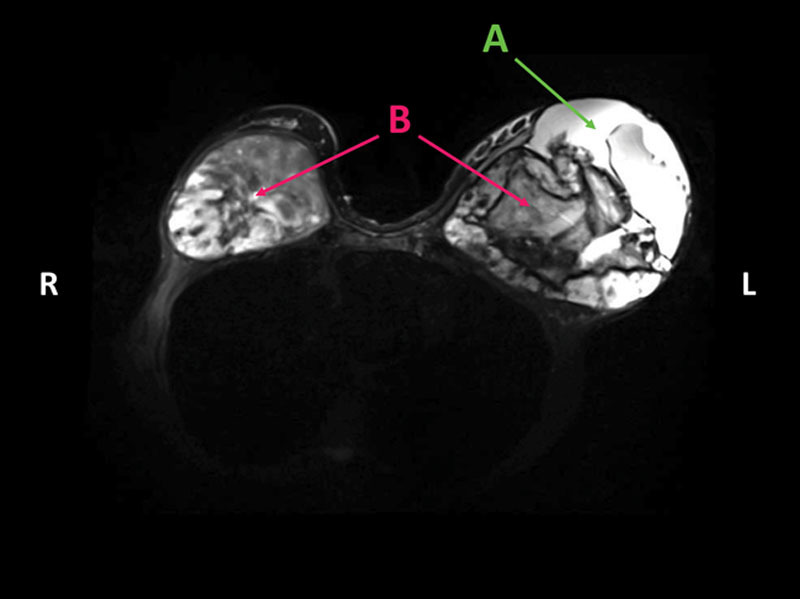
Magnetic resonance imaging of the breasts demonstrated large, heterogeneous, oval-shaped masses within the retropectoral spaces bilaterally, concerning for malignancy (Fig. 2). There was also evidence of a fluid collection within the left breast. T1-weighted magnetic resonance images of the right hemithorax showed areas of abnormal high signal intensity, consistent with extracapsular silicone implant rupture extending into the right axilla and upper extremity (Fig. (Fig.2).2). Due to initial suspicion of malignancy, a core biopsy was performed on the inferior left breast mass, which demonstrated benign pathology consistent with an organized hematoma.
The patient was taken to the operating room for bilateral implant removal and total capsulectomy. Complete rupture of the right implant was found, with extrusion of silicone material through the right axilla and upper extremity. An organized hematoma containing fibrinous material and silicone granulomas was evacuated from the right breast, with a total volume of approximately 200 mL. The extruded silicone was removed through an incision within the right bicipital groove (video below). In the left breast, a ruptured 300 cc silicone implant was found inside a fibrous capsule. A large volume of organized hematoma (~600 cc) was removed piecemeal from the inferior aspect of the left breast, and the hyperemic overlying skin was discarded. Bilateral gross specimens were sent for final pathology, both showing benign hematoma with scattered granulomatous reaction; specific staining for anaplastic large-cell lymphoma was negative. All incisions were closed primarily, with drains placed into each breast pocket.
Postoperatively, the patient received 4 units of packed red blood cells due to significant blood loss during the hematoma removal, but otherwise recovered well with no acute events or evidence of hemodynamic instability. At follow-up 1 month later, the patient was doing well, with no further complaints or complications (Fig. 4).
Authors
Riley A. Dean, BS,1Adam D. Glener, MD,1Analise B. Thomas, MD,1Steven R. Glener, BS,1Silvia Kurtovic, MD,1 and Detlev Erdmann, MD, PhD, MHSc
References
REFERENCES
- Handel N, Garcia ME, Wixtrom R. Breast implant rupture: causes, incidence, clinical impact, and management. Plast Reconstr Surg. 2013;132:1128. [PubMed] [Google Scholar]
- Brown SL, Silverman BG, Berg WA. Rupture of silicone-gel breast implants: causes, sequelae, and diagnosis. Lancet. 1997;350:1531. [PubMed] [Google Scholar]
- Hölmich LR, Friis S, Fryzek JP, et al. Incidence of silicone breast implant rupture. Arch Surg. 2003;138:801. [PubMed] [Google Scholar]
- Austad ED. Breast implant-related silicone granulomas: the literature and the litigation. Plast Reconstr Surg. 2002;109:1724; discussion 1731. [PubMed] [Google Scholar]
- Capozzi A, Du Bou R, Pennisi VR. Distant migration of silicone gel from a ruptured breast implant. Case report. Plast Reconstr Surg. 1978;62:302. [PubMed] [Google Scholar]
- Puckett MA, DeFriend D, Williams MP, et al. A leaking breast prosthesis presenting as an abdominal mass. Br J Radiol. 2004;77:790. [PubMed] [Google Scholar]
- Yoo H, Shin SJ, Park MC. Migration of a ruptured, silicone gel-filled breast implant into sternal and abdominal areas. Arch Aesthetic Plast Surg. 2014;20:178. [Google Scholar]
- Dragu A, Theegarten D, Bach AD, et al. Intrapulmonary and cutaneous siliconomas after silent silicone breast implant failure. Breast J. 2009;15:496. [PubMed] [Google Scholar]
- Hirmand H, Hoffman LA, Smith JP. Silicone migration to the pleural space associated with silicone-gel augmentation mammaplasty. Ann Plast Surg. 1994;32:645. [PubMed] [Google Scholar]
- Stevens WM, Burdon JG, Niall JF. Pleural effusion after rupture of silicone bag mammary prosthesis. Thorax. 1987;42:825. [PMC free article] [PubMed] [Google Scholar]
- Taupmann RE, Adler S. Silicone pleural effusion due to iatrogenic breast implant rupture. South Med J. 1993;86:570. [PubMed] [Google Scholar]
- Ahn CY, Shaw WW. Regional silicone-gel migration in patients with ruptured implants. Ann Plast Surg. 1994;33:201. [PubMed] [Google Scholar]
- Anderson DR, Schwartz J, Cottrill CM, et al. Silicone granuloma in acral skin in a patient with silicone-gel breast implants and systemic sclerosis. Int J Dermatol. 1996;35:36. [PubMed] [Google Scholar]
- Foster WC, Springfield DS, Brown KL. Pseudotumor of the arm associated with rupture of silicone-gel breast prostheses. Report of two cases. J Bone Joint Surg Am. 1983;65:548. [PubMed] [Google Scholar]
- Huang TT, Blackwell SJ, Lewis SR. Migration of silicone gel after the “squeeze technique” to rupture a contracted breast capsule. Case report. Plast Reconstr Surg. 1978;61:277. [PubMed] [Google Scholar]
- Mason J, Apisarnthanarax P. Migratory silicone granuloma. Arch Dermatol. 1981;117:366. [PubMed] [Google Scholar]
- Masson CL, Dessapt B, Rochet M. [Migration of silicone gel after rupture of a breast prosthesis during an external capsulotomy]. Ann Chir Plast. 1982;27:369. [PubMed] [Google Scholar]
- Persellin ST, Vogler JB, 3rd, Brazis PW, et al. Detection of migratory silicone pseudotumor with use of magnetic resonance imaging. Mayo Clin Proc. 1992;67:891. [PubMed] [Google Scholar]
- Sanger JR, Matloub HS, Yousif NJ, et al. Silicone gel infiltration of a peripheral nerve and constrictive neuropathy following rupture of a breast prosthesis. Plast Reconstr Surg. 1992;89:949. [PubMed] [Google Scholar]
- Teuber SS, Ito LK, Anderson M, et al. Silicone breast implant-associated scarring dystrophy of the arm. Arch Dermatol. 1995;131:54. [PubMed] [Google Scholar]
- Oh JH, Song SY, Lew DH, et al. Distant migration of multiple siliconomas in lower extremities following breast implant rupture: case report. Plast Reconstr Surg Glob Open. 2016;4:e1011. [PMC free article] [PubMed] [Google Scholar]
- Sagi L, Baum S, Lyakhovitsky A, et al. Silicone breast implant rupture presenting as bilateral leg nodules. Clin Exp Dermatol. 2009;34:e99. [PubMed] [Google Scholar]
- Baack BR, Wagner JD. Silicone gel breast implant rupture presenting as a fluctuant back mass after latissimus dorsi breast reconstruction. Ann Plast Surg. 2003;51:415. [PubMed] [Google Scholar]
- Collins JB, Verheyden CN. Incidence of breast hematoma after placement of breast prostheses. Plast Reconstr Surg. 2012;129:413e. [PubMed] [Google Scholar]
- Grippaudo FR, Renzi L, Costantino B, et al. Late unilateral hematoma after breast reconstruction with implants: case report and literature review. Aesthet Surg J. 2013;33:830. [PubMed] [Google Scholar]
Original source
Copyright
Copyright © 2018 The Authors. Published by Wolters Kluwer Health, Inc. on behalf of The American Society of Plastic Surgeons.This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal.


