Patient with giant upper limb melanoma
Abstract
A 57-year-old woman was referred to our regional sarcoma unit following a 2-year history of a progressively enlarging mass on her right forearm. At 14×7×12 cm, this mass turned out to be one of the largest upper limb cutaneous malignant melanomas ever described, and, to the best of our knowledge, the first documented in the UK. Remarkably, despite having a T4 malignant tumour with a Breslow thickness of 70 mm, this patient is still alive over 4 years later with no locoregional or distant metastatic spread. We present our experience in the management of this giant malignant melanoma of the upper limb and consider important differentials.
Case presentation
A 57-year-old woman was referred to our regional soft tissue sarcoma service with a large upper limb mass (figure 1). She had no medical history, however, she did have a family history of breast cancer; she worked as a cleaner. She presented late to her general practitioner, at 2 years, reporting of pain at the site of the lesion. The late presentation was due to extreme anxiety and avoidance of medical settings. On clinical examination, there was a large, pigmented, vegetating mass located on the extensor aspect of her right forearm. She had no sensory, motor or vascular deficits, and had a full range of elbow and wrist movements. Clinically, she had no palpable lymphadenopathy. The leading differential at presentation was that of soft tissue sarcoma.
Investigations
Initial work up of the mass was as per protocol for a potential upper limb soft tissue sarcoma. An initial MRI scan (figure 2) illustrated a 14×7×12 cm soft tissue mass on the ulnar aspect of the proximal forearm.
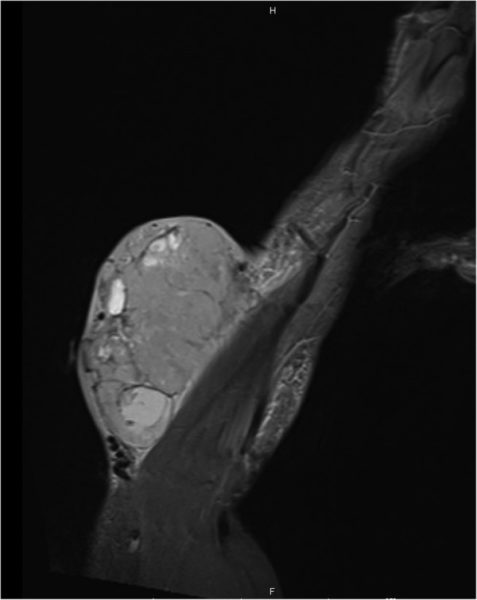
MRI showing large soft tissue mass at time of presentation.
An initial staging CT scan and a subsequent positron emission tomography scan showed several enlarged lymph nodes in the right axilla, likely reactive, but no other evidence of distant metastases. These were biopsied under CT guidance and found to be benign.
Differential diagnosis
There are a wide number of differentials to consider when approaching a large superficial soft tissue mass of the upper limb. It is important to consider and rule out soft tissue sarcoma early, and to refer to the regional sarcoma unit and multidisciplinary team (MDT) if clinical suspicion exists. Large lipomatous lesions are most commonly encountered.
Below is a summary, but not an exhaustive list, of other differentials to consider when investigating a large mass on the upper limb, adapted from a classification by Beaman et al.4
Mesenchymal
- Lipoma (very common in clinical practice)
- Dermatofibrosarcoma protruberans and liposarcomas
- Haemangiomas
- Nerve sheath tumours, for example, schwannoma and neurofibroma.
Skin
- Epidermal cyst
Metastatic
- Malignant melanoma, carcinoma and myeloma
Inflammatory
- Abscess
Other
- Myxoma, cutaneous lymphoma and granuloma annulare
Treatment
Preoperative core biopsies showed features consistent with malignant melanoma. A wide local excision, which included fascia and a cuff of extensor muscle bellies, was performed with curative intent. The defect was covered with a split skin graft from the thigh. At postoperative graft check, there was a 90% take. Such was the level of the patient’s anxiety and phobia of medical settings that she was not enrolled in the AVAST-M trial using the monoclonal antibody bevacizumab. This trial was for those deemed at high risk of recurrence from malignant melanoma.
Outcome and follow-up
Final histology showed a T4b, N0, M0 nodular malignant melanoma with a Breslow thickness of 70 mm and a Clark’s level of V. Further histological testing showed the tumour to be strongly positive for S100 and Melan-A (figure3), confirming the diagnosis of malignant melanoma. The nearest peripheral margin was 30 mm and the nearest deep margin was 0.5 mm, indicating complete surgical excision. This patient was followed up according to current UK Malignant Melanoma guidelines. Figure 4 shows her right forearm after excision and split thickness skin graft (SSG) 4 years after initial resection.
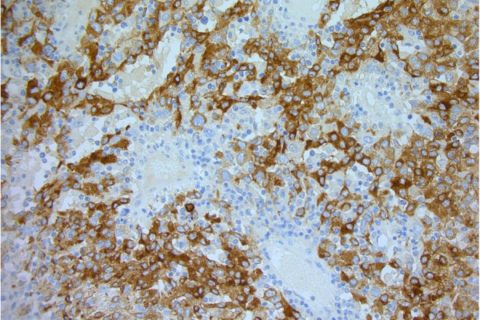
Histopathology image showing stain for Melan-A (×200).

Right forearm 4 years after initial excision and SSG.
Original Source
Authors
Department of Plastic Surgery, North Bristol NHS Trust, Bristol, UKCorrespondence to Calum Sinclair Honeyman,
Copyright 2016 BMJ Publishing Group Ltd
References
1. Cancer Research UK. Skin Cancer Incidence Statistics. http://www.cancerresearchuk.org/cancer-info/cancerstats/types/skin/incidence/uk-skin-cancer-incidence-statistics2. Ching A, Gould L. Giant scalp melanoma: a case report and review of the literature. Eplasty 2012;12:e51. [PMC free article] [PubMed] [Google Scholar]3. Harting M, Tarrant W, Kovitz C et al. Massive nodular melanoma: a case report. Dermatol Online J 2007;13:7. [PubMed] [Google Scholar]4. Beaman FD, Kransdorf MJ, Andrews TR et al. Superficial soft-tissue masses: analysis, diagnosis and differentials considerations. Radiographics 2007;27:509–23. 10.1148/rg.272065082 [PubMed] [CrossRef] [Google Scholar]5. di Meo N, Stinco G, Gatti A et al. Giant melanoma of the abdomen: case report and revision of the published cases. Dermatol Online J 2014;20:pii:13030/qt4pp2825w. [Google Scholar]6. del Boz J, García JM, Martinez S et al. Giant melanoma and depression. Am J Clin Dermatol 2009;10:419–20. 10.2165/11311050-000000000-00000 [PubMed] [CrossRef] [Google Scholar]7. Tseng W, Doyle J, Maguiness S et al. Giant cutaneous melanomas: evidence for primary tumour induced dormancy in metastatic sites. BMJ Case Rep 2009;2009:bcr07.2009.2073 10.1136/bcr.07.2009.2073 [PMC free article] [PubMed] [CrossRef] [Google Scholar]8. Marsden JR, Newton-Bishop JA, Burrows L et al. Revised U.K guidelines for the management of cutaneous melanoma 2010. Br J Dermatol 2010;163:238–56. 10.1111/j.1365-2133.2010.09883.x [PubMed] [CrossRef] [Google Scholar]9. Thomas JM, Newton-Bishop J, A’Hern R et al. Excision margins in high-risk malignant melanoma. N Engl J Med 2004;350:757–66. 10.1056/NEJMoa030681 [PubMed] [CrossRef] [Google Scholar]10. Grisham AD. Giant melanoma: novel problem, same approach. South Med J 2010;103:1161–2. 10.1097/SMJ.0b013e3181f3d756 [PubMed] [CrossRef] [Google Scholar]11. Zettersten E, Sagebiel RW, Miller JR III et al. Prognostic factors in patients with thick cutaneous melanoma (>4 mm). Cancer 2002;94:1049–56. 10.1002/cncr.10326 [PubMed] [CrossRef] [Google Scholar]
