Conquering the odds: Cirsoid aneurysm with holocranial feeders-staged embolization, excision and grafting
Authors: Sunil Munakomi, Binod Bhattarai, and Iype Cherian
A 38-year-old female presented with the complaint of slowly progressive swelling over scalp since last 20 years. There was no history of trauma, loss of consciousness, headache vomiting, altered sensorium or weakness of body parts. Surgical intervention was tried twice but abandoned due to heavy bleeding on both the occasions. On examination, there was a swelling of size 12 × 4 cm2 in the forehead and the scalp, which was slightly compressible with audible bruit over the swelling [Figures 1 and 2]. Magnetic resonance imaging (MRI) [Figure 3] and computed tomography (CT) revealed multiple dilated and tortuous vessels over the scalp in frontal and both temporal and parietal region with multiple collaterals. Right transverse, sigmoid and the jugular bulb were asymmetrically prominent.
Angiography revealed cirsoid aneurysm with feeders from external (superficial temporal, retroauricular and occipital), internal carotid (parasiting vessels from the callosomarginal arteries) and the left P2 VIA left vertebral arteries. Patient had undergone angiographic embolization of the feeders from the external carotid arteries as a staged procedure.
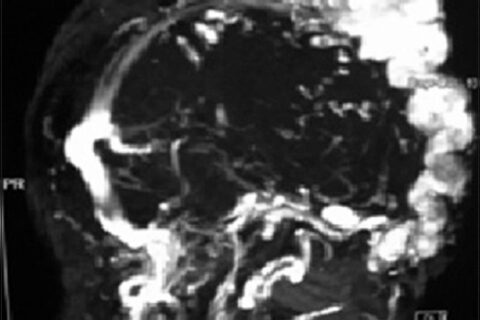
Magnetic resonance angiography
Care was taken to digitally compress the varix edges to prevent inadvertent embolic particle to enter the intracranial venous system. Ligation of remaining feeders and excision of varix with primary suturing of the scalp defect [Figure 6] was done 10 days later. Patient was started with Low molecular weight heparin and dextran to prevent propagating thrombus in the deep sinuses.
Postembolization and excision, CT scan showed no evidence of intracranial propagation of thrombus. Patient was subsequently taken up for skin grafting over the defect in the scalp due to ischemic edges of the defect (Figure 7). The patient made an uneventful recovery. Postoperative angiography showed only feeders from left occipital branch supplying the scalp.



