Acute esophageal necrosis
Introduction
Acute Esophageal Necrosis Syndrome (AENS) is a rare and unknown clinical entity, defined as a diffuse circumferential black-appearing friable esophageal mucosa going from the distal esophageal mucosa to the gastroesophageal (GE) junction. Esophagogastroduodenoscopy (EGD) remains the gold standard in making diagnosis.
Case Report
A 45-year-old man, with history of biliopancreatic diversion for alcoholic chronic pancreatitis, was referred to the emergency unit of Pasteur Hospital in Nice for a 72-h history of tiredness, dysphagia and hematemesis. There was no history of peptic ulcer disease or esophageal reflux and he denied ingestion of any caustic agents. On admission, there was no clinical sign of anemia and vital signs were in normal ranges, the patient was afebrile. Blood sample showed an inflammation syndrome with a white blood cell count at 10.8 × 109/L and a CRP measured at 128.0 mg/L. An emergency EGD was then performed and full necrosis of the lower esophagus was diagnosed (Fig. 1).
No bleeding site was identified. Microscopically, biopsies reported a full thickness necrosis of the esophagus wall without any extension to sub-mucous or muscular tissues. In the meantime, the patient experienced a cardiac arrest with generalized seizures. He was immediately transferred to the intensive care unit and medical management consisted of sedation, intubation and ventilation. A cervico-thoraco-abdominal computed tomography scan was completed characterizing stagnant fluid all long esophagus, duodenal wall thickening, liquid collection posteriorly to the duodenum and infiltration of fat tissue. No pneumoperitoneum nor pneumomediastinum were seen (Fig. 2). An endoscopic follow-up performed at day one confirmed circumferential necrosis of the esophagus, expanding from 25 of the dental arches to 45 cm, with no complications. The GE junction remained healthy with a sharp transition where the mucosa returns to its normal pink appearance. Biology samples displayed an inflammatory syndrome as well as an acute renal failure with creatinine at 239 μmol/L. Conservative management was decided after a multidisciplinary meeting. Extubation was possible at day 3 and the patient was placed on total parenteral nutrition. The patient was discharged at day 10, with parenteral nutrition and double-dose proton pump inhibitors (PPI). The patient did well and parenteral nutrition was stopped after a total duration of three weeks. Repeated endoscopic follow-up showed a global improvement however residual ulcerations with lower esophageal stricture were seen at one month. Iterative balloon dilation helped improve his clinical condition. Up-to-date, the patient is doing very well and does not require any further endoscopic treatment.
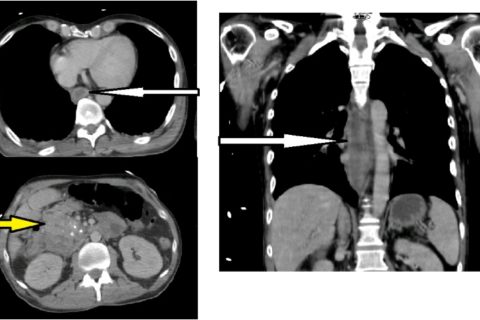
CT-scan with stagnant fluid in esophagus (white arrow) and thickening of the duodenal walls (yellow arrow).
Discussion
AENS is a rare clinical entity and thus has little mention in literature. This syndrome concerns more often elderly men, with a mean age of 67 years old . The etiology remains uncertain and is mainly multifactorial with the principal factors being low blood flow, diminished mucosal defenses and aggression of the esophageal mucosa by massive gastric content inflow . The most common risk factors are heart failure, atherosclerosis, diabetes, renal failure, drugs and cancer. In addition, acute conditions can also be responsible, such as sepsis, congestive heart failure, lactic acidosis, severe bleeding, severe pancreatitis, hypoalbuminemia, hypothermia, low blood pressure or any other trauma or shock . In our case, the patient was already known for alcoholic chronic pancreatitis, and during his stay, presented a cardiac arrest with severe sepsis and acute renal failure. It is the gathering of these factors that can lead to the development of AENS.
