Small bowel obstruction secondary to mobile phone ingestion: A minimally invasive approach to retrieval
CASE REPORT
A 34-year-old man ingested a mobile phone while on temporary release from prison. Five days later he began to develop acute severe periumbilical abdominal pain. This was associated with constipation, although he was passing small amounts of flatus. He vomited multiple times. He alerted prison officers to his ingestion of the phone and was transferred to his local hospital where he underwent initial management and investigation and was later transferred to a tertiary referral unit for definitive management.
His medical history was significant for previous open appendicectomy in childhood. He had no history of previous foreign body ingestion. He denied thoughts of self-harm, grandiose delusions, and auditory hallucinations. He had no previous psychiatric history or psychiatric admissions. He denied previous history of drug abuse. He was a current smoker with a 20 pack-year history.
On examination in the emergency department, he was found to have suprapubic and periumbilical tenderness with mild distension. He did not have signs of localized peritonism. He was vitally stable except for a mild tachycardia at 94 beats per minute.
Investigations
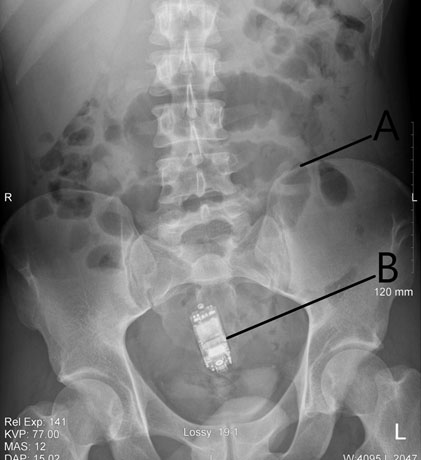
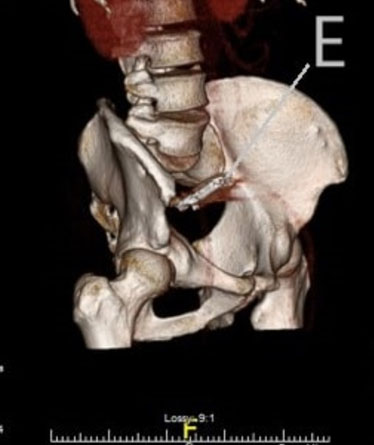
Lactate was within normal range at 1.4 mmol/L. His white cell count was mildly elevated at 11.48 × 109/L, predominantly a neutrophilia of 9.56 × 109/L. All other blood tests were within normal reference ranges. Plain film abdomen indicated a foreign body in the lower abdomen (Figure 1). There was no free air visible under the diaphragm on chest X-ray. Computed tomography of the abdomen and pelvis (CT AP) showed a distal small bowel obstruction with strong suspicion for transition point at the site of the ingested mobile phone level in the distal small bowel located within the pelvis (Figure 2 and Figure 3). The phone was described as being located in the midline, anterior to the sacral promontory, within the distal small bowel. The ileum was collapsed distal to this point. There were no signs perforation or intra-abdominal collection.
Differential Diagnosis
Given the patient’s clinical picture and radiological findings, the patient was diagnosed with a small bowel obstruction secondary to foreign body ingestion. It was decided that the patient should be transferred to the tertiary referral center for ongoing management of his condition with a view to definitive surgical management the next day.
Treatment
Due to the location of the phone in the distal small bowel, an attempt at endoscopic retrieval was not a viable option. Conservative management was deemed inappropriate due to both the clinical presentation of the patient with abdominal tenderness and the finding of distal small bowel obstruction on CT AP. The decision was therefore made to proceed with surgical retrieval of the phone. It was decided to manage the case similar to that of a gallstone ileus. Following informed consent the patient was transferred to the operating room for emergency exploration.
The patient underwent general anesthetic and was placed in supine position. A single 1.2 g dose of amoxicillin/clavulanic acid was given at induction. A longitudinal 10 mm port site was sited inferior to umbilicus via the Hasson technique. Two additional 5 mm ports were placed in the left iliac fossa and left flank under direct vision. Initial intraperitoneal findings showed dilated and decompressed small bowel loops. The cecum, appendiceal stump, and terminal ileum were identified in the right iliac fossa. Starting at the terminal ileum, a small bowel walk was performed in order to locate the mobile phone. The mobile phone was found in the distal jejunum. There was a clear transition from dilated to collapsed small bowel. Overlying bowel appeared edematous, however, there were no signs of necrosis or perforation. Two noncrushing bowel graspers were placed both distal and proximal to the foreign body. The infraumbilical port site was converted into a 3 cm lower midline mini laparotomy. An AlexisTM (Applied Medical, CA, USA) wound protector was deployed. The bowel containing the foreign body was delivered through the laparotomy site. A longitudinal isoperistaltic enterotomy on the antimesenteric surface of the bowel was formed to facilitate retrieval of the phone. The phone was found to measure approximately 6 × 1.5 cm and was wrapped in plastic (Figure 4 and Figure 5). Due to the healthy appearance of the distal bowel, primary transverse closure of the enterotomy was carried out in two layers with continuous mucosal 3/0 vicryl and interrupted seromuscular 3/0 Maxon sutures. The fascia was closed with round body 0 loop Maxon and skin was closed with 4/0 Monocryl. Twenty milliliters of 0.25% bupivacaine were administered at the port sites. There were no intraoperative complications and the patient returned to the ward to complete his recovery.
Outcome and Follow-up
The patient received standard postoperative intravenous antimicrobial prophylaxis. Mechanical and pharmacological thromboprophylaxis were administered. His diet was incremented gradually over the initial three days. He was noted to have passed a bowel motion on day 2 postoperatively. The patient had an uncomplicated postoperative course and was discharged back to prison five days after his operation. He was followed up in the clinic as an outpatient and was found to be very well. He was subsequently discharged from the surgical unit.
