Anticoagulant-induced priapism progressing to penile gangrene: a devastating complication!
Case presentation
A 35-year-old man, non-diabetic, non-hypertensive, married, having two children with normal erectile function, presented 4 h after sustaining gunshot injury to the left side of chest and left upper limb (figure 1). There were no injuries to the external genitalia. On evaluation, he had left pneumo-haemothorax which was relieved with insertion of intercostal chest tube and left upper limb ischaemia due to laceration of the brachial artery with thrombosis (confirmed by colour Doppler of left upper limb). His preoperative haematological parameters showed haemoglobin 13.2 gm/dl, total white blood cell (WBC) count 8200 cells/cmm3 and a normal differential WBC count. Platelet counts were 3 80 000 cells/cmm3. Coagulation parameters were within normal range (bleeding time 4 min, coagulation time 6 min 10 s and international normalised ratio (INR) 1.0). He underwent embolectomy with repair of the brachial artery using saphenous vein graft. Postoperatively, injection dalteparin (fragmin) 5000 IU subcutaneous (SC) twice daily along with oral warfarin 5 mg twice daily was started
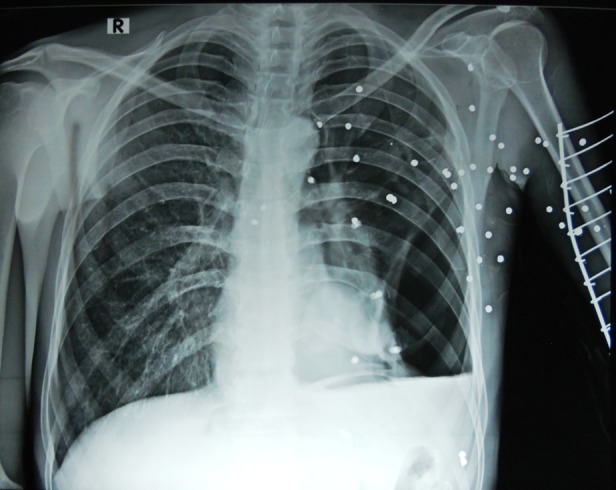
Chest x-ray showing pellets from gunshot injury causing left hemopneumothorax.
On the third postoperative day, the patient complained of penile pain with persistent erection of 12 h. Colour Doppler of penis showed low arterial flow and absence of venous flow. Coagulation parameters showed prothombin time was 137 s (control: 14 s) and INR of 9.8. In view of raised INR, anticoagulants were stopped immediately. Aspiration of cavernosal blood revealed dark, unclotted blood and analysis of cavernosal blood aspirate was consistent with ischaemic priapism. Coagulation parameters were corrected with transfusion of fresh frozen plasma and injection vitamin K given for 3 days, and the INR reached 1.2 the next day. Priapism was initially managed with repeated irrigation and aspiration followed by creation of distal cavernoglanular shunt (Winter shunt). Partial detumescence was achieved. But, 48 h from the onset of priapism, the glans started developing gangrene.
The patient was later referred to us after 7 days from the onset of priapism, dry gangrene had progressed till the peno-scrotal junction (figure 2). The urinary bladder continued to be drained by previously placed perurethral Foley catheter. Haematological work-up ruled out sickle cell disease or haematological malignancy. His platelet counts were marginally low (150 000 cells/cmm).

Penile gangrene till the peno-scrotal junction.
After counselling, informed consent was taken to perform total penectomy as enough penile stump could not be saved so as to enable him void in a standing position. Intraoperatively, there was dry gangrene till the peno-scrotal junction with thrombus extending proximally into the corpora cavernosal till the crural bifurcation. Corpus spongiosum was also thrombosed till the bulb of the penis.
Treatment
Total penectomy with perineal urethrostomy was performed after taking informed consent from the patient (figure 3). The left upper limb could not be salvaged and developed gangrene for which a mid-forearm amputation was done.

Total penectomy with perineal urethrostomy.
Outcome and follow-up
Postoperatively, the wound remained healthy and he is voiding well at 6 months of follow-up.
Abstract
Priapism by definition is full or partial erection that continues more than 4 h beyond sexual stimulation and orgasm or is unrelated to sexual stimulation.
A 35-year-old man developed priapism with the use of low-molecular-weight heparin and warfarin following repair of left brachial artery sustained after gunshot injury. Priapism progressed to penile gangrene despite decompression and distal shunt procedure leading to total penectomy and perineal urethrostomy. We describe the mechanism of anticoagulant (heparin and warfarin)-induced penile gangrene and the possible methods to avert such a devastating complication.
Background
Anticoagulants (like warfarin and low-molecular-weight heparin) are commonly used for the treatment of arterial and venous thrombosis to prevent clot propagation. They are also used to prevent thromboembolism in patients with thrombophilia, atrial fibrillation, mechanical heart valves and after high-risk surgery. In the setting of vascular thrombosis, both heparin and warfarin are initiated with warfarin being continued till the desired time. Strict monitoring is required to prevent overdose and avert unusual complications such as bleeding and rarely priapism. It is also known that both of them cause priapism individually.1 2 When used in combination it is difficult to pinpoint to the perpetuator of priapism. Priapism progressing to penile gangrene secondary to use of anticoagulant is still rare with only few cases being reported in the literature. Herein we report an unusual complication of penile gangrene after the use of anticoagulants.