Complete avulsion of the scalp by a rotating machine
Case Report
A 42-year-old woman presented to the clinic 28 h after complete avulsion of her scalp by a rotating machine. Her scalp had been simply sutured in situ without anastomosis in a local hospital within 3 h after injury. After another 16 h of monitoring, there were no signs of improved perfusion in the scalp, so the patient was transferred to their hospital for salvage surgery. The patient was clearly conscious with stable vital signs. On physical examination, the avulsed scalp involved almost the entire hairy scalp and forehead, sparing the occipital region in the nuchal area (Fig. 1). An ophthalmic examination revealed normal eye movements and pupil light reflexes. The laboratory tests showed an elevated white blood cell count (15.6 × 109/L, normal range 3.5–9.5 × 109/L) and absolute neutrophil count (11.7 × 109/L, normal range 1.8–6.3 × 109/L), indicating stress and acute inflammatory status. The patient also had mild anemia (90 g/L).
After the onset of anesthesia, the patient was maintained in the supine position. The amputated flap was shaved and cleaned. The right temporal vessels, left supratrochlear vein, and left supraorbital artery were identified and carefully dissected out of the recipient area. Then, corresponding vascular stumps were identified and trimmed in the amputee. End-to-end anastomosis was performed between vessels in the recipient area and counterparts area with vein grafts from the forearm (Fig. 2). The total operative time for anastomosis was 7 h, limiting the overall warm ischemia time to 35 h.
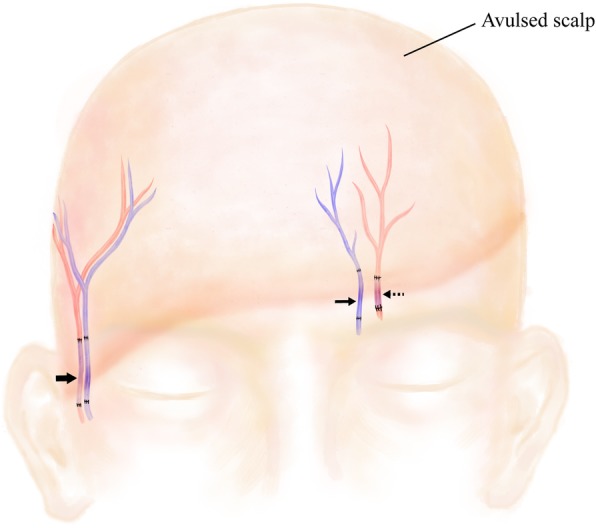
Schematic diagram of the microsurgical anastomosis of vascular stumps with vein grafts. (Bold arrow) The right temporal artery and vein; (arrow) the left supratrochlear vein; (dashed arrow) the left supraorbital artery
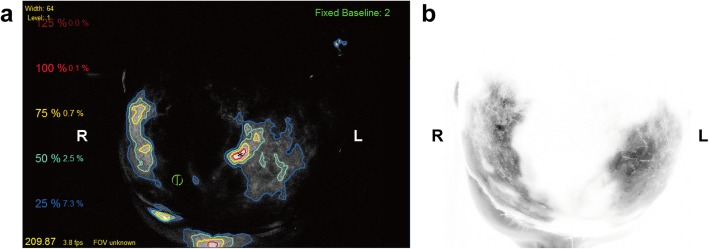
The entire scalp appeared well perfused, was flush red in color, and had positive pinprick bleeding and restored capillary refill (Fig. 3a, b). To confirm tissue perfusion, ICGA was conducted according to a previous study. Briefly, a 2-mL ICG bolus (2.5 mg/mL, Dandong Yichuang Pharmaceutical Co., China) was injected through a peripheral intravenous line.
Unfortunately, partial necrosis occurred 1 week later and became matured in 1 week. Tissue perfusion was assessed again with ICGA mapping, which showed a wide range of hypoperfused frontoparietal areas with a pattern in accordance with the intraoperative ICGA mapping results (Fig. 4b). The patient underwent major debridement surgery, during which we confirmed that the necrotic area correlated accurately with the hypoperfused areas that had less than 25% of maximal perfusion revealed by ICGA mapping at the time of replantation using quantitative SPY-Q analysis (Fig. 4a and Fig. 5).
Split skin grafting was performed with grafts from the back. All grafts survived, and the patient recovered uneventfully. Acceptable cosmetic results were achieved at the 1-month follow-up (Fig. 6). The patient was satisfied with her final appearance.
Author information
1Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital, Shanghai JiaoTong University School of Medicine, 639 Zhizaoju Road, Shanghai, 200011 People’s Republic of China
2Plastic and Reconstructive Surgery, Changzheng Hospital, Navy Military Medical University, Shanghai, People’s Republic of China
Tao Zan, Email: zantaodoctor@yahoo.com ;.Corresponding author.
#Contributed equally.
Copyright
Copyright © The Author(s) 2019Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.



