Facial gunshot wound – Successful recovery
A 60-year-old game-keeper with a medical history of mild depression presented to his local primary care centre with a high-velocity GSW to his face, following an attempted suicide with a shotgun. The practice immediately called for an ambulance and the air ambulance and ground team were mobilised. The first responder was at the scene 7 min after the call and air ambulance arrived 33 min after the call. At the scene, the patient was maintaining his own airway.
He maintained a Glasgow Coma Scale (GCS) of 15/15 and required no analgaesia. He was brought via air ambulance to the Queen Elizabeth Hospital, Birmingham, which is a major trauma centre. The patient arrived 1 h and 18 min after the first call. He was sat upright with his head extended for comfortable breathing.
Airway intervention was not necessary at the scene nor in the accident and emergency (A&E) resuscitation department. Figures 1 and and 2 show the patient maintaining his airway in the A&E resuscitation department. They also demonstrate the extensive tissue damage to the left hand side of the patient’s face.

Figure 1. The extent of tissue damage to the left side of the patient’s face can be seen. Note that the lateral aspect of the patient’s tongue is completely exposed and the left side of the mandible is absent.

Figure 2. The patient maintains his airway during initial resuscitation. Note the full thickness skin flap including part of the patient’s mandible protruding from under the lower half of the mask. The integrity of this tissue allowed this part of the mandible to be fixed back into position using a small plate, and the skin was salvaged to allow a good amount of primary wound closure.
At the major trauma centre, the patient was received by a trauma team with the addition of ear-nose-throat (ENT) and maxillofacial surgery doctors. A primary survey was performed and the patient then taken to theatre 1 h and 31 min after the first call to the ambulance. In theatre, a surgical tracheostomy was performed. The mandible was fixed, and primary closure was performed. The subsequent CT scan is shown in figure 3.
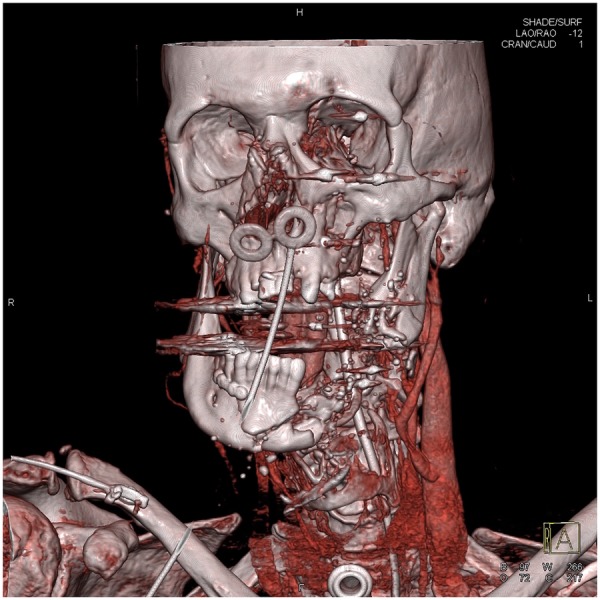
Three-dimensional CT reconstruction image showing tracheostomy, bilateral nasopharyngeal and nasogastric tubes in satisfactory position. The small plate used to fix a mandibular fragment in place can be seen (the same mandibular fragment is shown displaced in figure 2). The image also demonstrates the large defect remaining on the left side of the patient’s mandible. There are multiple other bony fractures. Shotgun fragments can also be seen within the soft tissue.
Treatment
On-scene management, resuscitation and stabilisation were performed, as described above. There was an open wound with discontinuity of the mandible on the left hand side, which could potentially threaten the patient’s airway. The patient was taken straight to theatre and a reconstruction plate used to stabilise the mandible allowing correction of the deformity and for soft tissue drape.
Following this, there were multiple trips to theatre for reconstruction with the intent of improving function and form. Day two postinjury, left midface wound debridement, intraoral wound washing, left eyelid foreign body removal and facial dressing were performed. At this point, anterior mandibular mucosa was blanching well. On day 7, the left side of the patient’s mandible was reconstructed with a plate. There was sufficient soft tissue over the plate and it was possible to achieve full mandible coverage using the patient’s own skin, as shown in figure 4. A skin graft was used to complete closure of the wound. Three weeks later, the patient was taken back to theatre for a dressing change and examination under anaesthesia. There was healthy granulation and satisfactory take of skin graft. A small dehiscence in the left neck, which did not communicate with the oral cavity, was packed with bismuth iodoform paraffin paste (BIPP) dressing. A small left cheek dehiscence with fistula oral cavity was freshened and closed with 3–0 vicryl. Intraoral examination showed healthy gingivae over the anterior mandible and no evidence of a neck fistula. Feeding continued through the naso-gastric route. One month and 4 days postinjury, the patient was discharged home. The appearance of the patient before nasal reconstruction and construction of a neomandible is shown in figure 5.

Figure 4. First of a series of images showing how the appearance of the injury improved throughout the management. A great deal of closure was achieved without the use of grafts. Soft tissue and skin cover of the mandible was achieved without the use of a graft. Nasogastric and bilateral nasopharyngeal tubes in position.
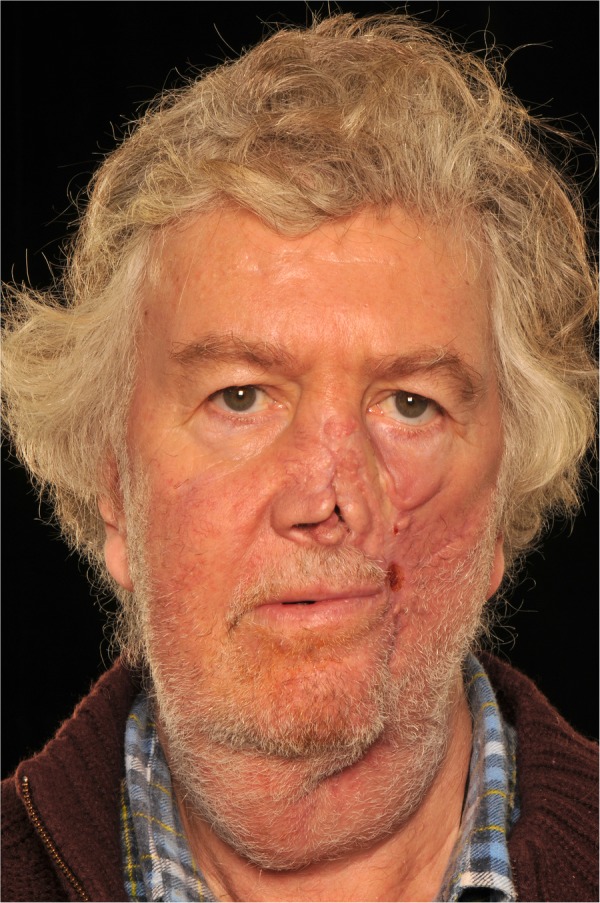
Three months after discharge, the patient returned to theatre for the first stage in a total reconstruction of his nose, using a paramedian forehead flap. As can be seen in figure 5, the right alar was intact, whereas the left alar was only partially intact with retraction and scarring. The nasal dorsum and lateral wall were absent with significant cheek scarring. Nasal subunits were marked and scar tissue was used as internal lining. The left cheek was undermined and medialised. Conchal cartilage grafts were used as dorsal and columellar struts and lower batton grafts bilaterally. The nasal bones were exposed, the deficient area was filled with cartilage and the irregular margins were rasped. A paramedian forehead flap was taken, thinned distally and sutured into place. The forehead was undermined and the glabella scored. Additionally, a dog-ear was excised within the hairline. On the same trip to theatre, an iliac crest bone harvest and construction of a neomandible were also performed. Grafts were cut with a NaCl-cooled saw and osteotome, and cancellous bone was harvested and bone wax applied. A left neck incision was made with dissection down to the reconstruction plate. The graft was trimmed with burr and fixed onto the reconstruction plate completing the neomandible.
In the following 3 months, the patient returned to theatre on two separate occasions for the final stages of nasal reconstruction. These involved pedicle division with tinning of the flaps followed by tissue undermining and debridement to create the alar crease.
Below is a summary timeline of the reconstruction.
- 19/11/13 Examination under anaesthesia, closure of facial wound, internal fixation of mandible, bilateral nasopharyngeal airway, temporary tracheostomy
- 21/11/13 Left midface wound debridement, left eyelid foreign body removal, facial dressing replaced
- 26/11/13 Left side of jaw reconstructed with plate
- 16/12/13 Examination under anaesthesia, head and neck wound redressed
- 23/12/13 Discharged home
- 19/03/14 First stage reconstruction of nose. Paramedian forehead flap. Iliac crest bone graft and construction of left neomandible
- 09/05/14 Second stage reconstruction of nose
- 21/07/14 Third stage reconstruction of nose
A multidisciplinary team was involved throughout the course of the patient’s treatment, although different specialties were added and subtracted as the treatment progressed. Teams involved included prehospital medical team/air ambulance, A&E, anaesthetics, trauma, multiple trauma service, psychiatry, maxillofacial surgery, plastic surgery, ophthalmology and ENT.
Outcome and follow-up
As can be seen from the series of images in figures 4-5, the appearance of the injury greatly improved throughout the management. At the time the photo shown in figure 5 was taken, the patient was being booked for an outpatient septorhinoplasty and his psychological state was also greatly improved.
He received psychiatric assessment on the intensive therapy unit (ITU) soon after his first trip to theatre, and was assessed as being low risk for a repeat attempt. The assessment revealed that he had recently undergone a marital separation but regretted the suicide attempt. He continued to be assessed during his stay in hospital before being discharged, when he moved back into his family home with his wife. Although the patient was assessed as low risk, the guns were removed from the property.