Giant Scalp Melanoma
Introduction: Among malignant melanoma lesions, those occurring on the scalp and neck have a particularly poor prognosis. In this case report, we present the largest melanoma of the head and neck and one of the largest melanomas of any anatomic site reported in the literature to date.
Case report
A 70 year old gentleman who initially presented for evaluation of a left scalp lesion (Fig 1). The lesion was present for 3 months, during which he had noted it increasing in size. Per patient report, it originally began as a small raised lesion above the left ear, which developed a dark streak heading posteriorly, and finally resulted in a 10×13 cm exophytic mass with irregular dark borders and scattered areas of ulceration. There was palpable lymphadenopathy, notably a left upper level 5 posterior cervical node of 3 cm in diameter and a left level 2 node of 4 cm in diameter. Biopsies from this first visit were consistent with nodular invasive malignant melanoma, Clark level V, Breslow’s thickness of at least 14 mm. A subsequent final needle aspiration of the enlarged lymph nodes was performed, revealing metastatic malignant melanoma. Computed tomographic scan showed invasion of the left parotid gland and cartilage of the left ear; however, there was no obvious cranial involvement by the lesion. A full workup for metastatic disease was completed, including computed tomography of the thorax, abdomen, and pelvis, which did not show any suspicious lesions. After discussion at institutional Tumor Board, the patient was preoperatively staged as T4aN3Mx. The patient inclined to pursue surgical resection of the lesion and selective left neck dissection.
Wide local excision with 3-cm margins was performed of the left scalp malignant melanoma, which included excision of the left ear en-bloc. There was a second lesion of the right scalp of 1×1 cm suspicious for malignant melanoma noted prior to surgery. An excisional biopsy was performed for the right scalp lesion and closed primarily during the same procedure. After excision of the scalp lesions was completed, a selective left neck dissection was performed. With the patient’s medical comorbidities and extent of disease, he was not a candidate for large flap reconstruction. Reconstruction with a Bilayer Wound Matrix (Integra, 311 Enterprise Drive, Plainsboro, New Jersey) was chosen to allow complete evaluation of the excisional margins of the scalp lesions prior to final closure of the defect with a thin split-thickness skin graft.
Results
Final pathology of the left scalp en-bloc excision revealed a 14.5 × 10.4 cm malignant melanoma, Clark level V, Breslow’s thickness of 18 mm, mitotic rate 35/mm2 (Figs 2 and 3). In addition, the right scalp lesion was a separate primary malignant melanoma. The neck dissection yielded 20 lymph nodes involved by metastatic melanoma out of 55 total lymph nodes examined. The anterior-inferior margin of the left scalp melanoma was involved; however, the patient declined to proceed with further resection. Final pathologic staging was determined to be T4b N3 M1, Stage IV.
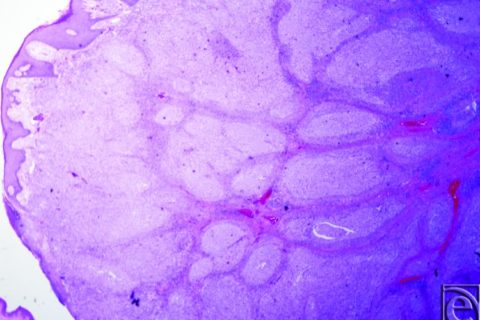
The lesion at 20× magnification.
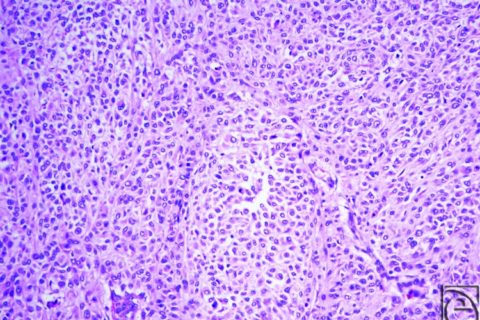
The lesion at 200× magnification.
Four weeks later, the patient was returned to the operating room for split-thickness skin graft placement on the left scalp acellular dermal matrix. The patient tolerated the procedure well, and the skin graft healed well with complete graft take (Fig 4).
Jessica A. Ching, MDa and Lisa Gould, MD, PhDb
aDepartment of Surgery
bJames A. Haley Veterans’ Hospital, University of South Florida, TampaCorrespondence: moc.liamg@gnihcnellaacissej

