Gross Hydrocephalus
Case Report
A 9-month-old second born child by normal delivery and cried immediately after birth with no perinatal complications presented with history of increasing size of head sine 4 months. On examination vitals were stable and drowsy with no cry Sun setting sign present, occipitofrontal circumference 65 cm, and (normal 32–35 cm conclusion hydrocephalus), weight 10 kg, dilated scalp veins. Both pupils were 3 mm reacting to light; visual acuity could not be assessed. No sensorimotor deficit except for spontaneous activity present in upper limbs more than lower limbs.
Lower limbs moving against gravity on pain stimuli [Figure 1]. Magnetic resonance imaging suggestive of tethered cord syndrome with Arnold chiari malformation Type II gross hydrocephalus with dilation of bilateral lateral ventricle, third ventricle and brain matter seen as mantle around ventricle [Figure 2] other investigations were normal. This baby posted for ventriculoperitoneal shunt surgery. In our case, the problems we anticipated were difficult intubation[1,2] due to presence of gross hydrocephalus, positioning of the baby for intubation and probability of hypothermia.[3]
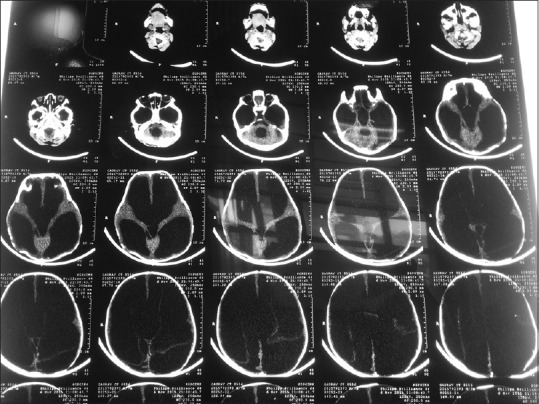
Magnetic resonance imaging of head (dilated ventricles, atrophy brain)
This baby has gross hydrocephalus so the difficult airway cart was kept ready. Though here the chances of difficult intubation were likely due to head size and positioning was difficult for intubation. After attaching all basic monitors induction done with sevoflurane 8% in incremental dial settings maintaining spontaneous respiration. Towel is kept below the shoulders to easy for intubation positioning. After checking for effective bag mask ventilation intravenous IV injection succinylcholine 2 mg/kg body weight given. Direct laryngoscopy done with Macintosh blade number 1, Cormack and Lehane grade (CLG) 3 with floppy epiglottis noted which was unable to lift up. First intubation attempt was failed.
Bag mask ventilation was done along with deepening the plane of anesthesia with sevoflurane. We immediately concluded it to be difficult airway. Second attempt of intubation was taken by the senior anesthesiologist along with the change of Macintosh blade number 2 and optimal external laryngeal maneuver, again there was no glottic visibility with similar difficulty. We continued with bag mask ventilation successfully in between ensuring oxygenation. Afterwards intubation attempt done with keeping towels below the shoulders properly and successful intubation achieved with 4 mm i.d. endotracheal tube (ETT) with little difficulty while negotiation [Figure 3].
Anesthesia was maintained on O2, air, sevoflurane, injection atracurium. 2.5 mg. Hemodynamic maintained stable, SpO2100, EtCO235 mmHg. Surgery lasted for 2 h. After the initiation of spontaneous respiration patient reversed with neostigmine and glycopyrrolate and was extubated carefully once the patient had protective airway reflexes and fully conscious [Figure 4]. Shifted to postoperative Intensive Care Unit for monitoring.
Author information
Department of Anaesthesiology and Critical Care, Sanjay Gandhi Postgraduate Institute of Medical Science, Lucknow, Uttar Pradesh, India
Address for correspondence: Dr. Raghavendra Vagyannavar, Room No. 336, New P.G. Hostel, Sanjay Gandhi
Postgraduate Institute of Medical Science Campus, Raebareli Road, Lucknow – 226 014, Uttar Pradesh, India. E-mail: moc.liamg@5002nlmuhgar
Reference
1. Bissonette B, Sadeghi P. Anaesthesia for neurosurgical procedures. In: Gregory GA, editor. Pediatric Anesthesia. 4th ed. Vol. 393. Edinburgh: Churchill Livingstone; 2002. pp. 4411–3. [Google Scholar]
2. Wheeler M. Management strategies for the difficult pediatric airway. Anesthesiol Clin North America. 1998;16:753. [Google Scholar]
3. Hooper VD, Chard R, Clifford T, Fetzer S, Fossum S, Godden B, et al. ASPAN’s evidence-based clinical practice guideline for the promotion of perioperative normothermia. J Perianesth Nurs. 2009;24:271–87. [PubMed] [Google Scholar]
4. Nienaber J. Anaesthesia for ventriculoperitoneal shunts. South Afr J Anaesth Analg. 2011;17:73–5. [Google Scholar]


