IMPALEMENT HEAD INJURY WITH A SPEAR
J West Afr Coll Surg. 2016 Apr-Jun; 6(2): 113–124.PMCID: PMC5342836PMID: 28344950
BI Akhiwu,AS Adoga, OP Binitie, CC Ani, M Iweagwu, O Adetutu,1T Ureme,1DD George,1PD Didamson,1E Oseni-Momodu,1 and BT Ugwu
Author information
Copyright and License information
Disclaimer
Case Reports
History
T.B was a 26-year old unemployed man who presented with a history of a spear thrown at him 6 hours prior to presentation.
He had gone at night to burgle a nearby restaurant and while trying to escape a spear was thrown on the face by a security guard. He escaped with the spare still attached to his face and he bled profusely from the nose and mouth but the bleeding had stopped before he presented to a nearby clinic. A good length of the wooden handle of the spear was sawn off before he was brought to Bingham University Teaching Hospital, Jos, Nigeria. There was no loss of consciousness or other systemic complaints. He was not a known diabetic, hypertensive or psychiatric patient but admitted to smoking marijuana habitually.
On presentation
he was fully conscious, but in painful distress with a locally made spear consisting of a metallic blade and a partially sawn off wooden handle penetrating obliquely from the right side of his nasal bridge just below the medial canthus with about 6cm length of blade exiting just below the left ear with crusts of blood in the nostrils and over the skin of the left parotid region (Figs. 1 & 2). No active bleeding was observed and there was limited mouth opening.
He was not pale, febrile, cyanosed, or dehydrated and his pulse rate was 80bpm, regular, full volume with a BP of 130/90mmHg. His respiratory rate was 24cpm, regular with stuffy nostrils containing crusts of dried blood and he used his mouth to breathe; his oxygen saturation was 92% in room air. There were no other significant systemic findings.
The admitting diagnosis
was impalement injury to the face. The patient was then admitted to the intensive care unit of the hospital and had the following investigations: skull x-rays, haematocrit, white blood cells and differentials, grouping and cross matching of 3 units of blood and computerized tomographic scan. He was promptly resuscitated and rehydrated, and appropriate antibiotics and tetanus toxoid administered.

Fig. 1
The entry point of the spear
Fig. 2
The exit point of the blade of the spear
CT brain scan
shows a sharp pointed object of metallic density traversing the face in a linear diagonal trajectory, entering through the right aspect of the nasal bridge, crossing the midline and the roof of the left maxillary sinus, below the inferior orbital margin and above the left supramandibular notch, before exiting below the left zygomatic arch. The left maxillary sinus is filled with isodense hemosinus. The cranium and its contents and the left mandible are spared.
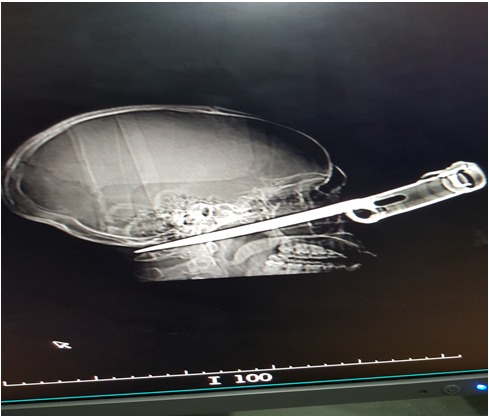
Pre-operative skull x-ray of the patient
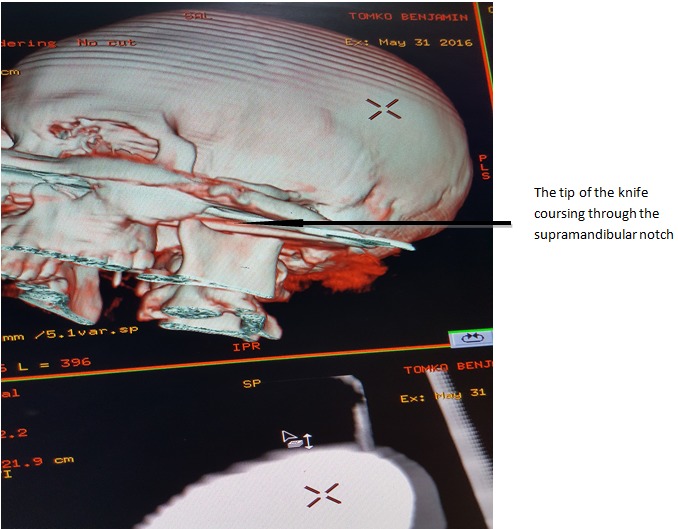
Brain CT scan (volume rendering image) showing the course of the knife through the skull
The operation was carried out by a team of surgeons consisting of a maxillofacial surgeon, an otorhinolaryngologist, a neurosurgeon and a general surgeon after an elective tracheotomy was first performed out under local anesthesia. Thereafter, the foreign body was traced from its entry in the right nasofrontal region where it was observed to transverse the left maxilla to fracture the zygoma and then pass through the supramandibular notch to exit at the inferior pinna region.
Prior to the skin incision, the superior labial vessels were ligated, and intravenous Dycemone 500mg and 8mg of dexamethasone were administered. A left Weber-Fergusson-Blair incision was made down to the facial bone to expose the hemi-face. Torrential bleeding was encountered from the anterior and posterior ethmoidal vessels at the entry point of the knife which was arrested by ligating the vessels with 3.0 Vicryl.
Bleeding was also noticed from the right maxillary antrum. Nasal anstrostomy was done; the right antrum was packed with ribbon gauze impregnated with povidone iodine while the left was packed with Merocoel to achieve hemostasis. Surgicel was used to enhance hemostasis from the bleeding bony edge of the nasal bridge. Intraoperatively the incisions were closed using 3-layered suturing using vicryl 3.0 while proline 4.0 was used for the skin.
The immediate post operative vital signs were as follows: pulse rate of 110/min, blood pressure of 140/82 mmHg, respiratory rate of 24 cycles per minute. The estimated blood loss was 300mls; one unit of whole blood was transfused intra-operatively. Post operatively he had his vital signs monitored every 15 minutes until he became fully conscious. The tracheostomy cuff was deflated for 5mins every hour and then re-inflated and deflated completely after 24 hours, suctioned when necessary and bicarbonate was instilled into the tracheostomy as required. The gauze in the right nostril was removed on the 4th post op day. Active mouth exercise was commenced within 24 hours using a wooden spatula and chewing gum. The patient was then placed on intravenous 5% dextrose/saline to alternate with normal saline for the first 72 hrs. He was also placed on ocular chloromphenicol twice daily.
On the 1st postoperative day he was observed to be stable with moderate facial oedema, the mouth opening was limited to one finger breath with good interdigitation of occlusion. He was commenced on supervised mouth exercise with wooden spatula and chewing gum, warm saline mouth rinse 7 times a day. He progressively improved and was discharged home on the 14th post-operative day after removal of the tracheostomy tube on the 7th day post-op without respiratory distress.

Fig. 5
The patient intra-operatively showing Weber-Fergusson-Blair incision and preservation of the infra orbital nerve

The impalement object

Fig. 7
The patient on the first day post operatively

Facial profile of the patient 2 weeks after surgery
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342836/