Necrotizing Scleritis
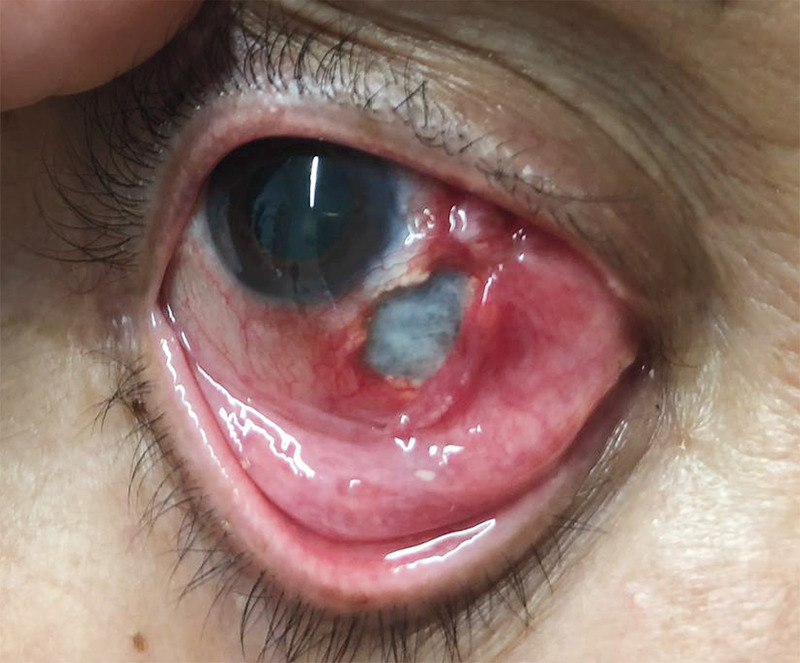
A 73-year-old woman with a history of seropositive erosive rheumatoid arthritis presented to the emergency department with a 1-month history of pain in her right eye. Four years before presentation, she had stopped her immunosuppressive treatment and switched to homeopathic therapies. The visual acuity was 20/25 in the affected eye. Slit-lamp examination showed hyperemia, inflammation, and marked scleral thinning with exposure of the underlying choroid. Laboratory studies showed an elevated level of rheumatoid factor, an increased erythrocyte sedimentation rate, and negative results on testing for antineutrophil cytoplasmic antibodies. A diagnosis of necrotizing anterior scleritis with inflammation was made. Treatment with intravenous glucocorticoids and cyclophosphamide was initiated, and the patient underwent surgical repair with a scleral graft and amniotic membrane transplantation. The patient also received a conjunctival autograft from the same eye. She completed a tapered course of an oral glucocorticoid, and immunosuppressive therapy was switched to oral methotrexate. At the follow-up visit 3 months after surgery, the ocular inflammation and pain had resolved and the patient’s vision was preserved.
Natalia Lorenzana Blanco, M.D.
Nicolas Alejandre Alba, M.D., Ph.D.
Hospital Universitario Fundación Jiménez Díaz, Madrid, Spain