Physician-Perceived Impact of Thyroid Eye Disease on Patient Quality of Life in the United States
Abstract
Introduction
Thyroid eye disease (TED) is an autoimmune disease that causes retro-orbital inflammation and subsequent proptosis, corneal exposure, strabismus, and variable vision changes. European studies have shown that TED can severely impact quality of life (QOL), but little is known about the QOL of patients with TED in the USA. Given that patient QOL influences TED severity classifications and subsequent treatment, understanding physician-perceived patient QOL is extremely important.
Methods
This retrospective chart review (conducted in 2018) examined QOL in US patients with moderate-to-severe TED, as reported by treating physicians who regularly manage patients with TED (≥ 5 patients in prior 12 months). The physicians graded patients’ overall QOL (7-point Likert scale; 1 = “not at all impaired”, 7 = “extremely impaired”), assessing mental health, vision changes, and ocular structural signs/symptoms. Patient demographics and clinical findings were examined to understand the impact of disease presentation on physician-perceived QOL.
Results
Medical record data of 714 US patients with moderate-to-severe TED were provided by 181 physicians (73 endocrinologists, 108 ophthalmologists). Patients had a mean age of 49.4 (standard deviation [SD] 13.6) years, and 102 cases (14%) were severe. Anxiety and/or depression was reported in 36% of patients (an increase from the 18.9% prevalence reported for the USA in 2017 by the US National Institute of Mental Health; P < 0.001). The mean physician-reported QOL impact score was 4.1 (SD 1.5). Furthermore, 62 and 89% of patients with moderate and severe TED, respectively, had a high physician-perceived QOL impact (≥ 4). The higher QOL impact group had significantly higher rates of pain symptoms, visual disturbances (including diplopia), and orbito-facial structural changes. Higher disease activity and severity were associated with lower physician-perceived QOL.
Conclusion
Patients’ QOL, as evaluated by US physicians, is highly impacted by the activity and severity of TED. Additionally, mental health issues were more frequently reported by patients with TED than in the general US population. Ocular pain, strabismus, and diplopia appear to be main drivers of physician-perceived QOL impairment in this sample of US patients with TED.
Plain Language Summary
Little is known on how thyroid eye disease (TED) affects patient quality of life (QOL) in the USA. Patient QOL can affect how TED is treated; consequently, it is important to understand how physicians perceive QOL in patients with TED. We evaluated 714 patients, as reported by physicians, with this rare condition to better understand QOL in US patients with TED. The medical records of 612 patients with moderate TED and 102 patients with severe TED were examined. QOL impact was rated from 1 to 7, with 1 being “not at all impaired” and 7 being “extremely impaired.” Overall QOL, as assessed by treating physicians, is heavily impacted by both moderate and severe TED in US patients, with these patients also reported to have a higher frequency of mental health diagnoses than reported in the general US adult population. Higher levels of inflammation on and around the eye and more severe disease led to a higher QOL impairment. More specifically, pain, visual disturbances (including double vision), and changes to the face and tissues around the eye all negatively affected QOL.
Key Summary Points
| Why carry out this study? |
| Limited data exist on the impact of thyroid eye disease (TED) on quality of life (QOL) in US patients, particularly physician-perceived QOL which directly influences TED severity classification and treatment decisions. |
| This large-scale study of a rare condition sought to examine QOL in US patients with moderate-to-severe TED and to determine influencing factors. |
| What was learned from the study? |
| QOL is heavily impacted by both moderate and severe TED in US patients. |
| Higher disease activity and more severe disease were associated with a greater QOL impact, more specifically, orbital pain, visual disturbances (including diplopia), and orbito-facial structural changes. |
Introduction
Thyroid eye disease (TED) is an autoimmune condition that begins with progressive inflammation, frequently referred to as ‘active’ or ‘acute’ TED. Inflammation and/or expansion of orbital and retro-orbital tissues can lead to subsequent ocular pain, proptosis, diplopia, exposure keratopathy, and optic neuropathy [1, 2]. After approximately 1–3 years, TED becomes chronic and less active with varying levels of long-term sequelae, such as proptosis and diplopia [3, 4]. Only about 2% of patients with moderate-to-severe TED are ever considered to be free of TED [5], which will hopefully change with newer, more targeted therapies. Therefore, many patients experience significant changes in their quality of life (QOL) due to changes in their appearance, visual alterations, inability to cope, and mental/psychiatric manifestations [6–8]. Studies have shown that patients with TED have an equivalent or poorer QOL than patients with diabetes, emphysema, or heart failure [9].
The effect of TED on patient QOL has been widely studied in Europe. However, only a few studies have evaluated the impact of TED on patients’ QOL in the USA. Similar to results of European studies [10, 11], Bradley et al. [12] found impaired QOL in patients with TED, with diplopia being an influencing factor. Schotthoefer and Wallace [13] demonstrated QOL improvement following surgical correction of TED-related strabismus. Lastly, Paulsen et al. [14] found that dry eye disease, which is highly present in patients with TED, significantly lowers QOL.
To the best of our knowledge, no prior studies have examined how physicians in the USA perceive QOL in their patients with TED. QOL assessment can influence treatment decisions and patient–physician relationships, both of which are of particular importance for patients with TED because physician-perceived QOL helps define disease severity and provides justification for utilizing certain immunosuppressive, surgical, and/or biological therapies [15]. In the study reported here, we examined the impact of physician-reported QOL on patients with moderate-to-severe TED. Patient clinical data were also examined to better understand the drivers of QOL impact.
Methods
This study was given exempt status by the Western Institutional Review Board (Puyallup, WA, USA; registration no.: IRB00000533), waiving the requirement of informed consent. All study conduct adhered to the tenets of the Declaration of Helsinki of 1964, and its later amendments. Ophthalmologists and endocrinologists who completed the survey were reimbursed for their time.
Ophthalmologists and endocrinologists who regularly manage patients with TED (at least 5 patients within the prior 12 months) completed an online survey between 1 September and 31 December 2018 regarding their TED patient population and treatment practices. Physicians were then asked to complete data collection forms (only de-identified data collected) using clinical records of up to four patients with moderate-to-severe TED. The survey forms also included questions on physicians’ perceptions on how TED impacted patient QOL, such as “To what degree does TED impair this patient?”, in terms of overall QOL and subscale measures (ability to attend work/school, ability to function in social situations, ability to participate and enjoy day-to-day activities, ability to drive and psychological well-being). Responses were scored using a Likert scale, ranging from 1 (“not at all impaired”) to 7 (“extremely impaired”). The survey was programmed in and administered via an established platform (Confirmit; Oslo, Sweden), and physicians were recruited from existing market research panels (via an independent third party [Biovid; Bristol, PA, USA]). A link to the screening questionnaire was sent via email to physicians. Those wishing to participate simply opted in by clinking on the link.
The median overall QOL impact was calculated and used as the cut-off point to divide patients into higher and lower QOL impact groups. Patient characteristics, pain, visual symptoms, and orbito-facial structural changes (e.g., proptosis, soft tissue changes, extraocular muscle involvement) were then compared between groups in an effort to understand how each of these factors potentially influenced QOL.
TED severity was reported by physicians as moderate or severe. TED activity for each patient was determined by calculating the clinical activity score (CAS), with 1 point given for each of the following signs/symptoms: pain in the primary gaze, pain with eye movement, eyelid swelling, eyelid redness, conjunctival swelling, conjunctival redness, and caruncle swelling [16]. In this survey, six of seven measures were used to calculate CAS because information on caruncle status was not available.
Statistical Analysis
Differences in patient and TED characteristics were compared using two-tailed chi-square tests for categorical variables (GraphPad QuickCalcs [online version]; Graphpad Software Inc., San Diego, CA, USA; accessed October 2020) and two-tailed Student’s t tests for continuous variables (Microsoft Excel, version 1808 [Office 2019 Professional]; Microsoft Corp., Redmond, WA, USA). Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using Microsoft Excel. Statistical significance was defined as P < 0.05.
Results
Physician Characteristics
A total of 899 physicians expressed interest in participating in the study. Of these, 183 (20%) met the inclusion criteria and completed the survey; 240 (27%) did not complete screening questions, 365 (41%) did not meet inclusion criteria, and 111 qualified physicians (12%) did not complete the survey. Two completed surveys did not meet quality control standards and were excluded. Therefore, surveys from 181 physicians were included in analyses.
Patient Characteristics
Physicians provided de-identified data on 714 patients who were diagnosed with moderate-to-severe TED. A total of 108 ophthalmologists reported on 432 patients (61%) and 73 endocrinologists reported on 282 patients (39%). Patient characteristics are summarized in Table Table1.1. Most patients were women (65%) and mean age at the time of data collection was 49.4 (standard deviation [SD] 13.6) years. Severe disease was reported in 102 (14%) patients. Overall QOL impact was 4.1 (SD 1.5) (median 4, range 1–7). There was no difference in mean overall QOL score between patients of endocrinologists (4.1 [SD 1.4]) and those of ophthalmologists (4.1 [SD 1.6]). At the time of data collection, 555 patients (78%) were euthyroid. A formal diagnosis of Graves’ disease was given in 487 patients (68%) and of Hashimoto’s thyroiditis in 25 patients (4%); 12 patients (2%) were diagnosed with both conditions.
Table 1
Characteristics of patients labeled as having moderate-to-severe thyroid eye disease
| Patient characteristics | All patients (N = 714) | Moderate TED (n = 612) | Severe TED (n = 102) | P valuea |
|---|---|---|---|---|
| Number (%) of patients of an ophthalmologist | 432 (61) | 370 (61) | 62 (61) | > 0.999 |
| Number (%) of women | 466 (65) | 398 (65) | 68 (67) | 0.835 |
| Age, mean (SD), years | 49.4 (13.6) | 49.5 (13.7) | 49.4 (12.7) | 0.949 |
| Number (%) of euthyroid patients | 555 (78) | 477 (78) | 78 (76) | 0.840 |
| Number (%) of patients with Graves’ disease | 487 (68) | 405 (66) | 82 (80) | 0.006 |
| TED duration, mean (SD), years | 4.2 (5.1) | 4.2 (5.1) | 4.2 (5.2) | 0.979 |
| Number (%) of patients with higher overall QOL impact (score ≥ 4) | 473 (66) | 382 (62) | 91 (89) | < 0.001 |
| Overall QOL impact score, mean (SD)b | 4.1 (1.5) | 4.0 (1.5) | 5.2 (1.3) | < 0.001 |
| Ability to attend work/school, mean (SD) | 3.5 (1.7) | 3.3 (1.6) | 4.8 (1.6) | < 0.001 |
| Ability to function in social situations, mean (SD) | 4.0 (1.6) | 3.8 (1.6) | 5.1 (1.4) | < 0.001 |
| Ability to participate in daily activities, mean (SD) | 3.8 (1.6) | 3.6 (1.5) | 5.0 (1.4) | < 0.001 |
| Ability to drive, mean (SD) | 3.6 (1.7) | 3.3 (1.7) | 5.0 (1.5) | < 0.001 |
| Psychological well-being, mean (SD) | 4.1 (1.5) | 3.9 (1.5) | 5.2 (1.3) | < 0.001 |
| Number (%) of patients with mental health issuesc | 260 (36) | 230 (38) | 30 (29) | 0.140 |
| Number (%) of patients with anxiety | 188 (26) | 174 (28) | 14 (14) | 0.003 |
| Number (%) of patients with depression | 131 (18) | 109 (18) | 22 (22) | 0.442 |
QOL Quality of life, SD standard deviaiton, TED thyroid eye disease
aComparisons of patients with moderate and severe TED were performed using a 2-tailed Student’s t test or chi-square test, as appropriate
bOverall and subscale QOL were scored by physicians using a Likert scale, ranging from 1 (not at all impaired) to 7 (extremely impaired)
cAnxiety and/or depression
Comparison of Patients with Moderate and Severe TED
Patients with severe TED had a significantly higher mean negative QOL impact score than those with moderate TED (5.2 [SD 1.3] vs. 4.0 [SD 1.5], P < 0.001). Additionally, 89 and 44% of patients with severe TED had an overall QOL impact score ≥ 4 and ≥ 6, respectively. Among those with moderate TED, 62 and 16% had an overall QOL impact score ≥ 4 and ≥ 6, respectively. All examined QOL subscales had a mean impact score of ≥ 3.5, with “psychological well-being” having the highest impact score (mean 4.1 [SD 1.5]). All subscale QOL measures were rated significantly higher in patients with severe TED than in those with moderate TED, indicating a perceived poorer QOL (Table (Table1).1). Diagnosis of anxiety and/or depression was noted in 260 patients (36%), with 188 patients (26%) having anxiety, 131 patients (18%) having depression, and 59 patients [8%] having both. Anxiety was significantly more prevalent in patients with moderate TED than in those with severe TED (28 vs. 14%, P = 0.003; OR 2.50, 95% CI 1.38−4.51, P = 0.001), but depression was similarly reported in both groups (18 and 22%, P = 0.442; OR 0.79, 95% CI 0.47−1.32, P = 0.182).
Effect of TED Signs and Symptoms on QOL Impact
Approximately two-thirds (66%) of patients were categorized into the higher QOL impact group (overall QOL score ≥ 4; Table Table2).2). Patient age and the proportion of women did not differ between the two groups, but duration of TED was shorter in the higher QOL impact group.
Table 2
Characteristics of patients with moderate-to-severe thyroid eye disease who had a higher and lower quality of life impact
| Patient characteristics | All patients (N = 714) | Overall QOL impact < 4 (n = 241) | Overall QOL impact ≥ 4 (n = 473) | P valuea |
|---|---|---|---|---|
| Number (%) of patients of an ophthalmologist | 432 (61) | 150 (62) | 282 (60) | 0.551 |
| Number (%) of women | 466 (65) | 157 (65) | 309 (65) | > 0.999 |
| Age, mean (SD), years | 49.4 (13.6) | 49.8 (14.5) | 49.2 (13.2) | 0.445 |
| Number (%) of euthyroid patients | 555 (78) | 185 (77) | 370 (78) | 0.728 |
| Number (%) of patients with Graves’ disease | 487 (68) | 162 (67) | 325 (69) | 0.749 |
| TED duration, mean (SD), years | 4.2 (5.1) | 5.0 (5.8) | 3.8 (4.7) | 0.006 |
| Clinical activity score, mean (SD)b | 2.3 (1.8) | 1.5 (1.5) | 2.7 (1.9) | < 0.001 |
| Number (%) of patients with severe disease | 102 (14) | 11 (5) | 91 (19) | < 0.001 |
| Number (%) of patients with mental health issuesc | 260 (36) | 77 (32) | 183 (39) | 0.092 |
| Number (%) of patients with anxiety | 188 (26) | 60 (25) | 128 (27) | 0.595 |
| Number (%) of patients with depression | 131 (18) | 35 (15) | 96 (20) | 0.075 |
aComparison between higher and lower QOL impact groups performed using 2-tailed Student’s t test or chi-square test as appropriate
bTED severity was reported by physicians as moderate or severe. TED activity for each patient was determined by calculating the clinical activity score (CAS), with 1 point given for each of the following signs/symptoms: pain in the primary gaze, pain with eye movement, eyelid swelling, eyelid redness, conjunctival swelling, conjunctival redness, and caruncle swelling. In this survey, data for caruncle swelling were not available and thus the CAS ranged from 1 to 6
cIndicates reporting of anxiety and/or depression
Mental Health Issues
Anxiety and depression were highly reported in both QOL impact groups (anxiety 25 and 27%, depression 15 and 20%; Table Table2).2). Patients were further stratified by overall QOL impact (groups 1–7 representing an overall QOL impact score of 1–7, respectively) to examine trends between overall QOL impact and anxiety or depression. The proportion of patients with reported anxiety was relatively steady across all QOL impact score groups, but depression progressively increased from 12% in group 1 (not at all impaired) to 25% in group 7 (extremely impaired).
Ocular Pain
Most ocular signs and symptoms of TED were reported more often in patients with a higher QOL impact score. Ocular pain symptoms associated with TED were significantly more prevalent in the higher QOL impact group than in the lower QOL impact group (photophobia 46 vs. 24%, OR 2.71, 95% CI 1.92−3.84; pain with eye movement 40 vs. 13%, OR 4.59, 95% CI 3.02−6.98; pain in primary gaze 30 vs. 9%, OR 4.36, 95% CI 2.70−7.04; all P < 0.001; Fig. 1a). However, discomforts associated with exposure keratopathy were equally and highly present in both QOL impact groups (ocular dryness/grittiness 85 and 84%; excessive tearing 60 and 56%; results not shown).
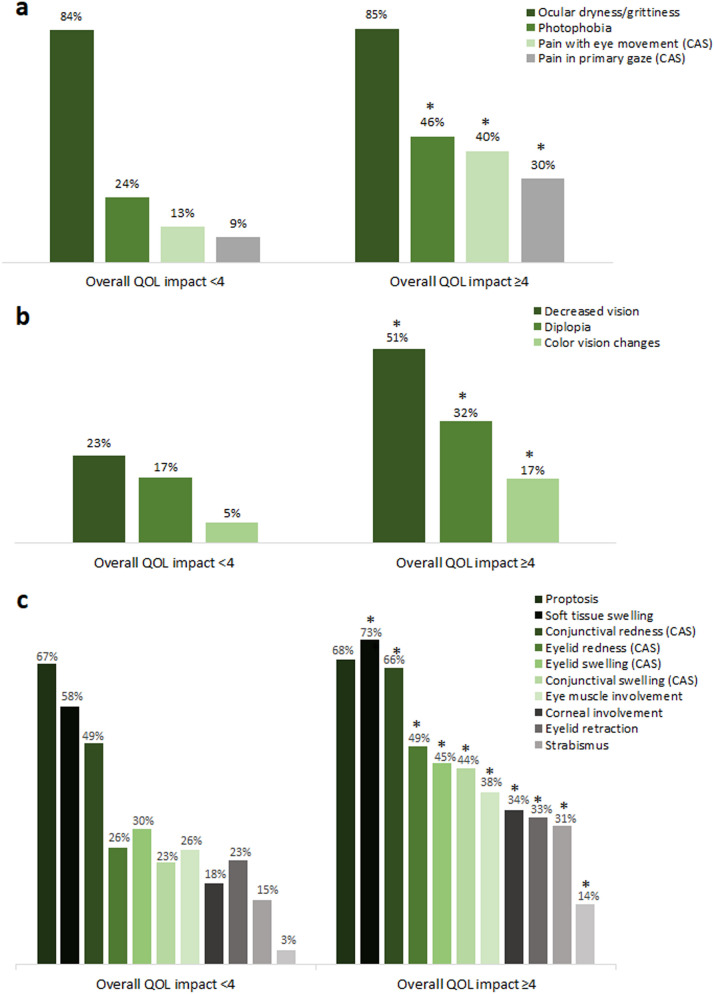
Prevalence of pain symptoms (a), vision-related symptoms (b), and structural signs (c) associated with thyroid eye disease in patients with a higher and lower quality of life (QOL) impact score. Asterisks indicate a statistically significant difference between groups as calculated using a 2-tailed chi-square test (a, b: all P < 0.001; c: all P ≤ 0.009). CAS Clinical activity score measure (see section “Methods” for details)
Vision-Related Symptoms and Structural Signs
All examined vision-related symptoms were significantly more prevalent in the higher QOL impact group than in the lower QOL impact group (all P < 0.001; Fig. 1b), including decreased vision (51 vs. 23%, OR 3.49, 95% CI 2.46−4.95), diplopia (32 vs. 17%, OR 2.27, 95% CI 1.54–3.33), and color vision changes (17 vs. 5%, OR 3.62, 95% CI 1.97−6.66). The structural signs and symptoms of TED were also examined and compared (Fig. 1c). With the exception of proptosis, which was equally and highly prevalent in both groups (67 and 68%), all structural signs were reported significantly more often in the higher QOL impact group than in the lower QOL impact group.
The proportion of patients with decreased vision (reported as decreased visual acuity, blurred vision, and/or vision loss) progressively increased from 15 to 75% as the overall QOL impact score increased from 1 to 7. Similar findings were observed for eye muscle involvement (from 24 to 75%). More specifically, reporting of diplopia increased from 21 to 57% and reporting of strabismus increased from 6 to 50% as the overall QOL impact score increased from 1 to 7.
Effect of TED Activity on Perceived QOL
Thyroid eye disease was more active in the higher QOL impact group (mean CAS: 2.7 [SD 1.9] vs. 1.5 [SD 1.5]; CAS ≥ 3: 53 vs. 23%, OR 3.74, 95% CI 2.63−5.30; all P < 0.001). Patients were grouped by CAS (range 0–6 [caruncle status not reported]) to further examine the influence of disease activity on QOL impact. The overall QOL impact score progressively increased with increasing CAS (Fig. 2).
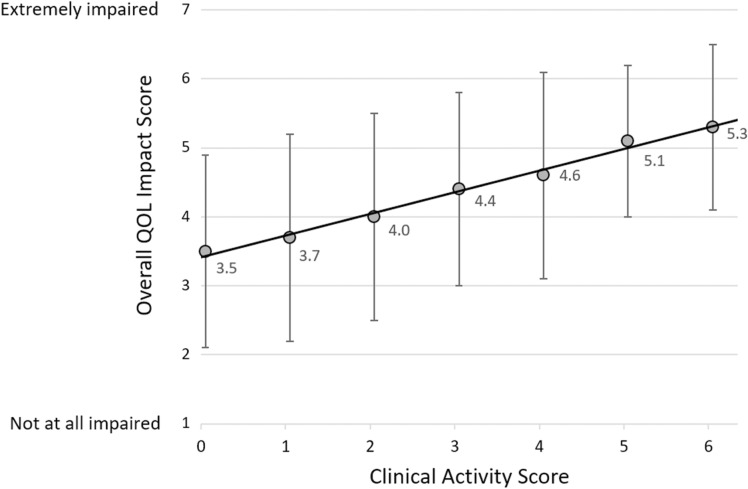
Relationship between the overall QOL impact score and CAS. The best-fit line is shown (y = 0.311x + 3.413, r = 0.375; 714 patients, P < 0.001). The CAS was calculated using six of seven measures because caruncle status was not reported. Data points represent mean overall QOL impact score and error bars represent 1 standard deviation
Patients with a higher QOL impact score reported all examined CAS components more frequently (Fig. 1a, c). This was particularly true of orbital pain (pain in primary gaze and/or with eye movement), which was reported nearly threefold more often in the higher QOL impact group (47 vs. 17%, OR 4.52, 95% CI 3.08−6.64; both P < 0.001).
Effect of TED Severity on Perceived QOL
Severe disease was reported more often in patients with a higher QOL impact score (Table (Table2).2). Furthermore, the proportion of patients with severe TED progressively increased from 0 to 54% as the overall QOL score increased from 1 (not at all impaired) to 7 (extremely impaired; Fig. 3). Although physicians made the determinations on TED severity, clinical parameters described by the American Thyroid Association (ATA) [16] and European Group on Graves’ Orbitopathy (EUGOGO) [15] that contribute to TED severity classifications were examined. Factors that progressively increased with overall QOL impact score included eye muscle involvement (24–75%), corneal involvement (18–61%), and the presence of compressive optic neuropathy (0–25%).

The proportion of patients with severe thyroid eye disease in patients at each overall QOL impact level. QOL impact was rated on a 7-point Likert scale with 1 = not at all impaired and 7 = extremely impaired. TED Thyroid eye disease
Source: https://www.ncbi.nlm.nih.gov/pmc/