Scalp expansion for giant cutis verticis gyrata secondary to cerebriform intradermal nevus
Wenfang Dong, Huan Wang, and Fei Fan
Case report
A 27-year-old woman was admitted to the hospital for evaluation of a huge black scalp macule (20 × 18 cm) with thinning of the overlying hair (Figure 1). The asymptomatic scalp macule first appeared upon her birth and gradually increased in size. On physical examination, the scalp macule was characterized by brain-like sulcus and gyrus formation, which is a typical feature of CVG, without other abnormalities. Normal results were obtained for all laboratory tests, including routine blood, urine, and stool analyses; hepatorenal function; blood glucose and lipid concentrations; and electrolyte concentrations. The patient’s medical and familial histories were unremarkable. The patient was diagnosed with secondary CVG. Because tumoral lesions are the most common cause of secondary CVG and because of the aesthetic concerns associated with the disease, surgical management was considered the optimal treatment.

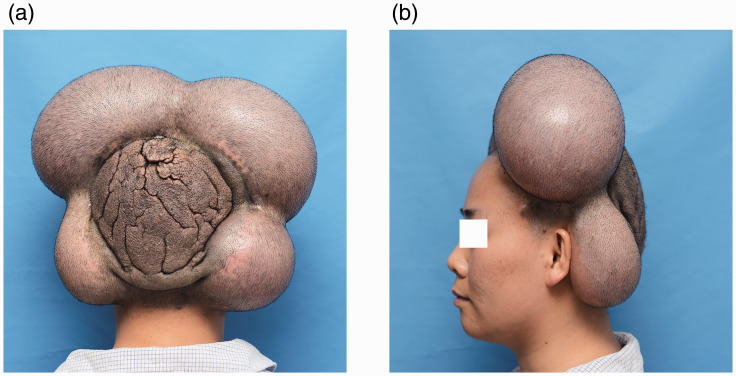
Four rectangular inflatable tissue expanders (300-, 300-, 100-, and 80-mL) were placed under the scalp galea on both sides of the forehead and mastoid regions and inflated twice weekly until they reached a total volume of 1400, 1400, 450, and 400 mL, respectively. (a) Occipital view of the cutis verticis gyrata (CVG) after scalp expansion. (b) Lateral view of the CVG after scalp expansion.
We were concerned that the patient did not have enough hair-bearing tissue for scalp reconstruction after surgical excision because of the extensive scope of the lesion. Therefore, a two-stage surgery with reconstruction was finally planned. During the first stage, four rectangular inflatable tissue expanders (300-, 300-, 100-, and 80-mL) were placed under the scalp galea on both sides of the forehead and mastoid regions (Figure 2). Over a 6-month period, the expanders were inflated twice weekly until they reached a total volume of 1400, 1400, 450, and 400 mL, respectively. During the second stage, full-thickness excision of the lesion with a 0.5-cm skin margin was performed without disturbing the periosteum, and closure was achieved with rotation advancement flaps from the adjacent expanded scalp without perioperative complications (Figure 3). The patient was diagnosed with CIN according to postoperative pathological findings. During the 6-month postoperative follow-up, there was no evidence of recurrence; only a scar was present under the coverage of the hair.
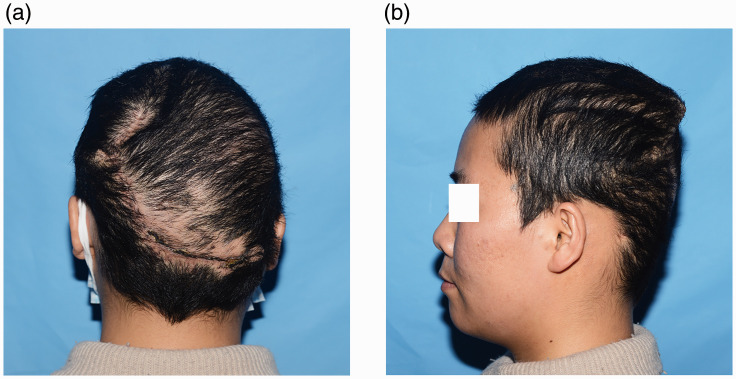
(a) Occipital view of the operation area 1 month after excision. (b) Lateral view of the operation area 1 month after excision.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Ethical approval: All procedures involving this patient were performed in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding: This work was supported by the CAMS Innovation Fund for Medical Sciences (Grant No. CAMS-12M-1-007).
Informed consent: Informed consent was obtained from the patient described in this report.
ORCID iD: Wenfang Dong https://orcid.org/0000-0002-5873-2517Go to:
References
1. Polan S, Butterworth T. Cutis verticis gyrata; a review with report of seven new cases. Am J Ment Defic 1953; 57: 613–631. [PubMed] [Google Scholar]2. Snyder MC, Johnson PJ, Hollins RR. Congenital primary cutis verticis gyrata. Plast Reconstr Surg 2002; 110: 818–821. [PubMed] [Google Scholar]3. Orkin M, Frichot BC, 3rd, Zelickson AS. Cerebriform intradermal nevus. A cause of cutis verticis gyrata. Arch Dermatol 1974; 110: 575–582. [PubMed] [Google Scholar]4. Zhang MJ, Sun ZY, Liu Y, et al. Rare giant secondary cutis verticis gyrata. J Plast Surg Hand Surg 2011; 45: 212–214. [PubMed] [Google Scholar]5. Hayashi Y, Tanioka M, Taki R, et al. Malignant melanoma derived from cerebriform intradermal naevus. Clin Exp Dermatol 2009; 34: e840–e842. [PubMed] [Google Scholar]6. Abu-Jamra F, Dimick DF. Cutis verticis gyrata. A report of a case secondary to acromegaly treated with plastic surgery and x-ray therapy. Am J Surg 1966; 111: 274–277. [PubMed] [Google Scholar]7. Garden JM, Robinson JK. Essential primary cutis verticis gyrata. Treatment with the scalp reduction procedure. Arch Dermatol 1984; 120: 1480–1483. [PubMed] [Google Scholar]8. Jeanfils S, Tennstedt D, Lachapelle JM. Cerebriform intradermal nevus. A clinical pattern resembling cutis verticis gyrata. Dermatology 1993; 186: 294–297. [PubMed] [Google Scholar]9. Hashimoto I, Urano Y, Nakanishi H, et al. Cerebriform intradermal nevus: a case of scalp expansion on the galea. J Dermatol 1999; 26: 258–263. [PubMed] [Google Scholar]10. Al-Malaq A, Hashem FK, Helmi A, et al. Surgical correction of primary cutis vertices gyrata. Ann Plast Surg 2002; 49: 673–675. [PubMed] [Google Scholar]11. Zhao L, Fang F, Xu J, et al. Giant primary cutis verticis gyrata successfully treated with surgical excision and tissue expansion. Dermatol Surg 2006; 32: 753–755. [PubMed] [Google Scholar]12. Wang MG, Chu YJ, Shui QF, et al. [Cutis verticis gyrata]. Zhonghua Zheng Xing Wai Ke Za Zhi 2007; 23: 112–114. [PubMed] [Google Scholar]13. Misirlioglu A, Karaca M, Akoz T. Primary cutis verticis gyrata and scalp reduction in one stage with multiple pinwheel flaps (revisited). Dermatol Surg 2008; 34: 935–938. [PubMed] [Google Scholar]14. Radwanski HN, Almeida MW, Pitanguy I. Primary essential cutis verticis gyrata–a case report. J Plast Reconstr Aesthet Surg 2009; 62: e430–e433. [PubMed] [Google Scholar]15. Hsu YJ, Chang YJ, Su LH, et al. Using novel subcision technique for the treatment of primary essential cutis verticis gyrata. Int J Dermatol 2009; 48: 307–309. [PubMed] [Google Scholar]16. Mishra A, Tehrani H, Hancock K, et al. Management of primary cutis verticis gyrata with tissue expansion and hairline lowering foreheadplasty. J Plast Reconstr Aesthet Surg 2010; 63: 1060–1061. [PubMed] [Google Scholar]17. Dumas P, Medard De Chardon V, Balaguer T, et al. [Primary essential cutis verticis gyrata: case report and literature review]. Ann Chir Plast Esthet 2010; 55: 243–248. [PubMed] [Google Scholar]18. Zhao D, Li J, Wang K, et al. Treating cutis verticis gyrata using skin expansion method. Cell Biochem Biophys 2012; 62: 373–376. [PubMed] [Google Scholar]19. Tagore KR, Ramineni AK. A case of cutis verticis gyrata secondary to giant cerebriform intradermal nevus. Indian J Pathol Microbiol 2011; 54: 624–625. [PubMed] [Google Scholar]20. Taha HM, Orlando A. Butterfly-shape scalp excision: a single stage surgical technique for cutis verticis gyrata. J Plast Reconstr Aesthet Surg 2014; 67: 1747–1749. [PubMed] [Google Scholar]21. Mutlu OO, Colak O, Canli M, et al. Scalp reconstruction with free latissimus dorsi flap in a patient with giant cutis verticis gyrata. J Craniofac Surg 2016; 27: e553–e554. [PubMed] [Google Scholar]22. Sahni K, Singh S, Bhari N, et al. Giant cerebriform intradermal nevus in a young girl. Indian Dermatol Online J 2016; 7: 443–444. [PMC free article] [PubMed] [Google Scholar]23. Lamelas AM, Taub PJ, Silver L, et al. Congenital primary essential cutis verticis gyrata. Eplasty 2016; 16: ic13. [PMC free article] [PubMed] [Google Scholar]24. Ennouhi MA, Guerrouani A, Moussaoui A. Idiopathic cutis verticis gyrata in a female. Cureus 2018; 10: e2105. [PMC free article] [PubMed] [Google Scholar]
Articles from The Journal of International Medical Research are provided here courtesy of SAGE Publications
Copyright © The Author(s) 2020Creative Commons Non Commercial CC BY-NC: This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
The Twelfth Department of Plastic Surgery, Plastic Surgery Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, ChinaFei Fan, The Twelfth Department of Plastic Surgery, Plastic Surgery Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, 33 Badachu Road, Shijingshan District, Beijing 100144, China. Email: nc.ude.cmup.hsp@iefnaf