Sterile subconjunctival abscess in an HLA-B51-positive patient with ulcerative colitis
Sterile subconjunctival abscess in an HLA-B51-positive patient with ulcerative colitis
Nobuyuki Kukimoto
aDepartment of Ophthalmology, Tokyo Metropolitan Tama Medical Center, Tokyo, Japan
Nanase Honda
bDepartment of Rheumatic Diseases, Tokyo Metropolitan Tama Medical Center, Tokyo, Japan
Naoto Yokogawa
bDepartment of Rheumatic Diseases, Tokyo Metropolitan Tama Medical Center, Tokyo, Japan
Akiko Ohno-Tanaka
aDepartment of Ophthalmology, Tokyo Metropolitan Tama Medical Center, Tokyo, Japan
Abstract
Purpose
To report a rare case of aseptic abscess presenting as a subconjunctival abscess in an HLA-B51-positive patient with ulcerative colitis.
Observations
A 25-year-old, male, Japanese patient with ulcerative colitis presented with an unilateral subconjunctival abscess. Infective endocarditis with endophthalmitis was suspected of being the cause, and systemic antimicrobial therapy was begun. The patient became critically ill and experienced the complication of heart failure with mitral valve perforation but improved dramatically with high-dose corticosteroids and intravenous infliximab following mitral valvuloplasty. His HLA typing was positive for HLA-B51.
Conclusions and importance
Both infectious and non-infectious etiologies should be considered in a patient with a subconjunctival abscess with systemic inflammation. An aseptic abscess can present as a subconjunctival abscess, and HLA-B51 may play a role in the pathogenesis of this rare condition.
1. Introduction
Subconjunctival abscesses are usually caused by a bacterial infection associated with a previous trauma or surgery or may be secondary to a systemic infection.1, 2, 3 Non-infectious etiologies are rarely reported but can occur spontaneously.4, 5, 6 Described herein is a case of an aseptic systemic abscess presenting as a sterile subconjunctival abscess associated with ulcerative colitis (UC) which was successfully treated with high-dose glucocorticoids and tumor necrosis factor alpha inhibitor.
2. Case report
A 25-year-old, male, Japanese patient was admitted for acute panuveitis accompanied by decreased vision in the right eye, which he discovered on waking. Ten days before onset, he visited a general ophthalmologist for redness in his right eye, general malaise, and fever. The ophthalmologist diagnosed uveitis and prescribed a steroid eye drop. The patient had no history of eye disease, injury or surgery but had received the diagnosis of UC six years ago and experienced a flare three months prior to the current admission. He was treated with mesalazine and tapered doses of prednisolone.
His best-corrected visual acuity was 20/200 in his right eye and 20/16 in his left eye. The right eye had ciliary hyperemia, anterior chamber inflammatory cells 4+, anterior chamber flare 4+, vitreous opacification 3+ according to the Standardization of Uveitis Nomenclature (SUN) criteria,7 and a subconjunctival abscess in the inferonasal area (Fig. 1). The subconjunctival abscess was attached to the sclera and had no mobility. His left eye was unremarkable. His body temperature was 38.2 °C, a pansystolic murmur was audible in the apex, and mild tenderness was noted in the left lower quadrant of the abdomen. A pustular rash was observed on the face and trunk (Fig. 2). Laboratory data showed elevated white blood cells (11,700/μL, neutrophils 83%, lymphocytes 9%) and C reactive protein (13.9 mg/dL). Transthoracic echocardiography showed severe mitral valve regurgitation due to anterior leaflet perforation with an aneurysm. Contrast-enhanced computed tomography (CT) visualized multiple lung nodules and multiple liver, splenic, intramuscular, and subcutaneous abscesses (Fig. 3). Neither CT nor magnetic resonance imaging revealed any intracranial or cervical lesions.
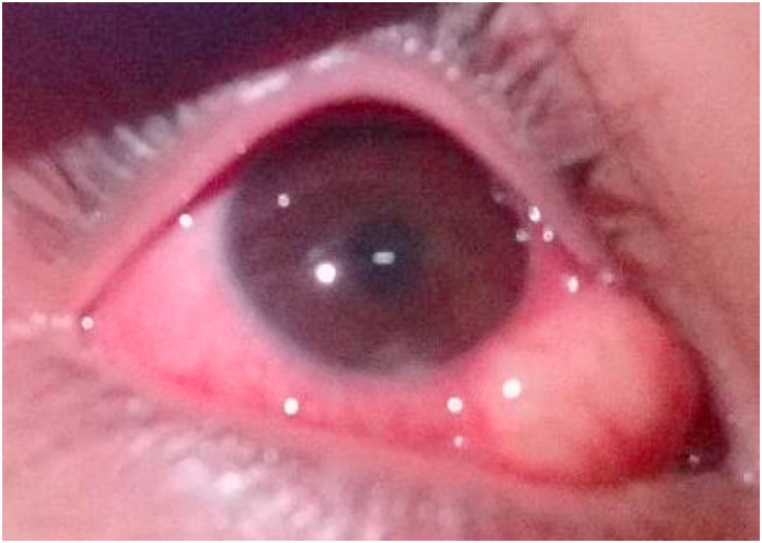
Photograph of the right eye. Examination of the right eye at presentation revealed ciliary hyperemia and a subconjunctival abscess in the inferonasal conjunctiva attached to sclera.

Photographs of patient face (Fig. 2A), chest (Fig. 2B) and back (Fig. 2C). Pustular rash on face and trunk on admission with no pain or itching.

Contrast-enhanced computed tomography on admission. Yellow arrows indicate lung nodules (Fig. 3A), liver abscesses (Fig. 3B) or intramuscular abscesses (Fig. 3C). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
An infection due to a pathogenic organism was thought to have caused the initial abscess, with secondary infections leading to the infective endocarditis and endogenous endophthalmitis with the subconjunctival abscess. However, Gram stain of fine needle aspiration specimens of the subconjunctival (Fig. 4), subcutaneous, and intramuscular abscesses was negative for bacteria and fungi. Furthermore, three sets of blood cultures were also negative for pathogenic organisms. Surgical intraocular fluid sampling was considered but was not performed because the sclera was thin and highly inflamed and the possibility of prolonged wound healing was a matter of concern.

Fine needle aspiration specimen of the subconjunctival abscess with opaque, yellowish-white coloration.
The subconjunctival abscess decreased in height and volume after the fine needle aspiration (Fig. 5), and no change was observed in the other lesions. However, the fever, systemic abscesses, and mitral valve regurgitation deteriorated.

Photograph of the right eye (on the day after the fine needle aspiration). The subconjunctival abscess decreased in height and volume after the aspiration.
Pathological analysis of the subcutaneous abscesses revealed neutrophil infiltration into the dermis and non-infectious abscess formation. In addition, neutrophil infiltration was also observed in the subcutaneous adipose tissue (Fig. 6), a condition known as neutrophilic panniculitis. Human leukocyte antigen (HLA) typing was positive for A11, A24, B51, and B52. Based on these findings and the unresponsiveness to antimicrobial therapy (vancomycin, ceftriaxone, metronidazole), the possibility of an aseptic abscess (AA) associated with UC was considered. After starting high-dose glucocorticoid therapy, including pulse doses from Day 13 and infliximab infusion from Day 22, the patient improved dramatically. The ocular inflammation improved significantly, and the corrected visual acuity returned to 20/20 in his right eye on Day 43. Optic disc swelling, which also improved gradually, was noted after the improvement in vitreous opacity. The sclera at the site of the subconjunctival abscess showed slight thinning, then stabilized(Fig. 7)without perforation. A detailed fundus examination revealed exudate deposition along the veins in the retina resembling local retinal phlebitis where the subconjunctival abscess was observed. Dye leakage was observed at the same site on fluorescein angiography.

Pathology specimen. Photomicrograph of subcutaneous tissue with neutrophil infiltration below the dermis and subcutaneous adipose tissue (so-called neutrophilic panniculitis).

Photograph of the right eye on Day 76 (after dilation). The synechia remained, but the other inflammation-related findings improved. The sclera in the area where AA was located (inferonasal area) was slightly thinned, and discolored grayish.
On Day 89, mitral valvuloplasty was performed, and on Day 125 the patient was discharged. The mitral valve had a perforation about 10 mm in size (Fig. 8).

Resected specimen of the part of the mitral valve with a roughly 10 mm perforation.
3. Discussion
We reported herein a rare case of non-infectious subconjunctival abscess occurring as a manifestation of aseptic abscess syndrome associated with ulcerative colitis. In a patient with a subconjunctival abscess with systematic inflammation, bacterial and fungal cultures of the abscess should be performed immediately to check for the presence of a systemic infection. If the result is negative, AA should be considered as a differential diagnosis, because AA sometimes causes heart valve perforation as in this case and can be fatal.13
AA, a rare autoinflammatory disease mainly affecting young adults, is characterized by recurrent fever and deep, round, aseptic lesions potentially involving all the organs. It is associated with inflammatory bowel disease (IBD),8,9 relapsing polychondritis,10 Behcet’s disease,10 neutrophilic dermatosis, such as pyoderma gangrenosum,11 and Sweet’s syndrome.12 As in the present case, AA can be complicated by extra-intestinal manifestations of IBD in which extensive microbiologic workups return negative, and patients are unresponsive to antimicrobial therapy. Relapses can be prevented by corticosteroid and immunosuppressive drug administration, such as TNF-α and IL-1 receptor antagonists.10,12 The present patient required infliximab in addition to glucocorticoid therapy to treat the inflammation. The dosage of the glucocorticoid was reduced as early as possible before surgery to avoid the risk of steroid-associated complications. Mitral valvuloplasty was then performed as soon as possible.
UC and Crohn’s disease (CD) are both forms of IBD that may have associated ocular symptoms, such as uveitis, scleritis, episcleritis, peripheral keratopathy, and posterior segment involvement, including pars plana exudates, vitreous inflammation, and retinal vasculopathy.14 An upper eyelid abscess in a patient with UC11 and a case of scleromalacia perforans in a patient with CD were also previously reported.15 The present case is the first instance of a subconjunctival abscess observed in association with IBD.
The pathophysiology of AA is unknown but may be related to genetic susceptibility. NOD2/CARD15, a susceptibility gene for CD, was analyzed in patients with AA with or without IBD, but no association was found.8 The association between AA and HLA typing, however, has never been investigated. HLA-B51 carries a high relative risk of Behcet’s disease, especially in patients with an ocular disease.9 The patient in the present case did not have any features of Behcet’s disease, such as oral or genital ulcers. However, HLA-B51 may have contributed to the development of his AA, and spontaneous activation of HLA-B51-positive neutrophils may have led to perivascular tissue injury and promotion of a Th1 immune response.
4. Conclusion
Both infectious and non-infectious etiologies should be considered in a case of subconjunctival abscess with systemic inflammation, especially if the patient has a history of autoimmune disease. A subconjunctival abscess can be a form of aseptic abscess, with HLA-B51 potentially playing a role in its pathogenesis.
Declaration of competing interest
None.
Acknowledgments
We are indebted to Dr. Motoyuki Hisagi and Dr.Takahiro Kiriu for their instruction and Mr. James R. Valera for his assistance in editing the manuscript.
References
Content retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7896157/.