Suicide attemp attempt with gun – Successful Recovery
A 24-year-old male defence personnel reported to the casualty department of our institution around 2:45 a.m. after a suicidal attempt by his service rifle during his night duty hours. The appearance was very horrific with total disfigured anatomy of the left half of his face [Figure 1].
His general medical condition was poor with vitals recorded as pulse-92/min, blood pressure-94/58 mm Hg and respiratory rate-16/min. He was agitated but appeared well-oriented. The patient was stabilized and on examination it was found that the point of entry of the bullet was from the submental region with a punctured wound and the exit site was in the left eye through the malar region. The tongue was bisected into two halves, with perforation of left maxilla and loss of dento-alveolar segment, ruptured nasal floor mucosa and total degloved left half of the mid face. He was bleeding from the oral and nasal cavity and the left side of his mid face. The left eye showed dilated pupil with no reaction to light and absence of vision. The right eye was with normal function. He was immediately shifted to the emergency operation theater. Debridement and primary repair of the wound was performed under general anesthesia [Figure 2].
His routine investigations, radiographs and computed tomography (CT) scans were performed. CT scan showed communited fracture of all the boundaries of the left orbit including maxilla, mandible and zygomatic bone [Figure 3]. A foreign body was seen in the infero-medial part of the left orbit and was referred to the Department of Ophthalmology. His left globe of the eye was found damaged and was exenterated [Figure 4]. After 1 week, open reduction and internal fixation of the fractured facial bones was performed along with maxillomandibular fixation for 6 weeks. The feeding was performed through nasogastric tube for 1 week followed by liquid diet for next 6 weeks.
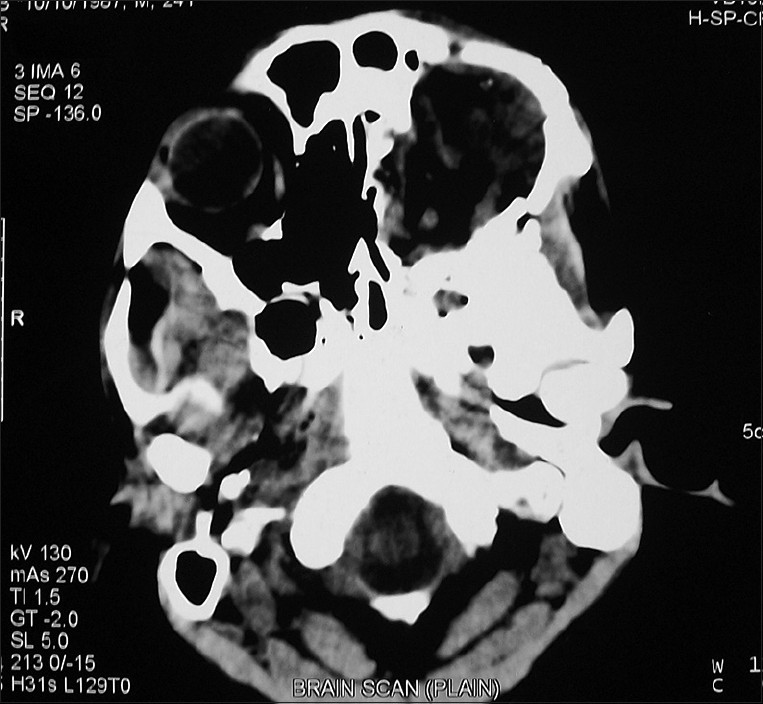
Figure 4: Axial view of computed tomography scan showing completely damage of the globe of left eye with fractured surrounding bones
After about 3 months, the patient reported to us with an unsatisfactory scar over the left mid face and he wanted the replacement of his lost eye [Figure 5]. On examination, it was noted that the left eye, upper and lower eyelids and partial maxilla of the left side were missing. An obturator was fabricated to facilitate speech and mastication. An intraoral and extraoral prosthesis was advised for rehabilitation of esthetics, speech and mastication for the patient. Obturator was made to facilitate speech, mastication and to separate the nasal and oral cavity. To prevent intrusion of material into the defect, a moist gauge pad with petroleum jelly, was applied. Mouth preparation was done. Impression for intraoral prosthesis was taken using irreversible hydrocolloid. The impressions were poured with Type IV die stone. Metal framework made up of Chrome-Cobalt alloy was fabricated.Inter-occlusal record, placement of teeth and wax finishing of prosthesis was done. Following wax up, flasking and dewaxing was done. It was acrylized using heat-cure acrylic resin. For extra oral impression the patient was instructed to sit in an upright position with a straight gaze ahead to minimize muscular movements.The impression was made using irreversible hydrocolloid (Algitex) and Plaster of paris. To prevent intrusion of material into the defect, a moist gauge pad with petroleum jelly was applied. Impression was poured with Type III dental stone. Placement of custom made eye-ball, wax finishing of both upper and lower eyelid along with maxilla. Finished wax pattern was trial inserted and invested. Color matching of silicone done by mixing with intrinsic stain (Cosmesil intrinsic silicone coloration system). Eye and silicone material (Cosmesil series silicone material, M511, both part A and part B) was put into the die after painting it with separating media. The die was clamped and placed at room temp for 24 h. Artificial eye lashes were placed. The prosthesis was retained with adhesive (Principality cream adhesive G602)[Figure 6]
The patient was advised to keep wound and prosthesis clean. He was advised to gently remove any exudates over the wound with a wet cotton tip soaked with 5% povidone-iodine solution and to clean the intaglio surface of prosthesis once daily with soap water. He was advised to come after 24 h for the adjustment of the obturator. Follow-up visits were done after a week, a month and 3 months post prosthesis insertion for further adjustment and correction.




