A Case of Ceftriaxone-Induced Acute Generalized Exanthematous Pustulosis/Generalized Pustular Psoriasis Overlap
Case Report
A 40-year-old man presented with pustular lesions all over the body for approximately 4 days’ duration. The onset of pustular lesions was accompanied by fever of a moderate degree and malaise. The patient admitted to unprotected extramarital contacts about a month and a half before the appearance of the pustular lesions. He stated that there was a small painless ulcer on the foreskin about 3 weeks before admission to our hospital, and the rapid plasma reagin card test was reported as reactive in a dilution of 1: 64 about 10 days before admission. He had been treated for primary syphilis with ceftriaxone for a duration of 10 days. However, the pustular lesions began appearing on the trunk on the sixth day after medical treatment and had spread to all body regions by the day of admission. Moreover, the patient mentioned that he had a history of psoriasis over a span of 20 years and had been treated with acitretin irregularly.
Physical examination revealed the presence of a generalized eruption of pustules on an erythematous base, which particularly involved the scalp, neck, trunk, and extremities (Fig. 1). The lesions were superficially loose pustules ranging from 2 to 20 mm in diameter and partial pustules dried up to form developed crusts on top of the ulcers. There were several asymptomatic erythematous lesions on both the palms and the soles of the feet. His mucous membranes, however, were not involved.

Fig. 1
Multiple pustular and crusted lesions on the trunk (a) and extremities (b, c) on the day of admission.
Laboratory data disclosed the following values: white blood cell count of 13,670/mm3, hemoglobin level of 11.4 g/100 mL, neutrophil absolute value of 9,540/mm3, and lymphocyte absolute value of 1,950/mm3. Syphilis serologic studies revealed that the toluidine red unheated serum test (TRUST) was reported as reactive in a dilution of 1: 32. Multiple cultures of the blood and the cutaneous pustules were done but all were negative. The HIV status of the patient was negative. Cerebrospinal fluid examinations for lymphocytosis, the venereal diseases reference laboratory test, and TRUST showed negative results.
A biopsy specimen taken from one of the crusted lesions 6 days after admission showed parakeratosis and minimal hyperplasia in an area of the epidermis. The dermis showed an inflammatory infiltrate, comprising lymphocytes and plasma cells (Fig. 2a, b). A biopsy specimen taken from one of the plaque lesions 12 days after admission showed parakeratosis and intraepidermal neutrophilic granulocyte abscess. A biopsy of the dermis showed telangiectasia in the dermis papilla, dermal superficial perivascular lymphocytes, and neutrophil infiltration (Fig. 2c, d).
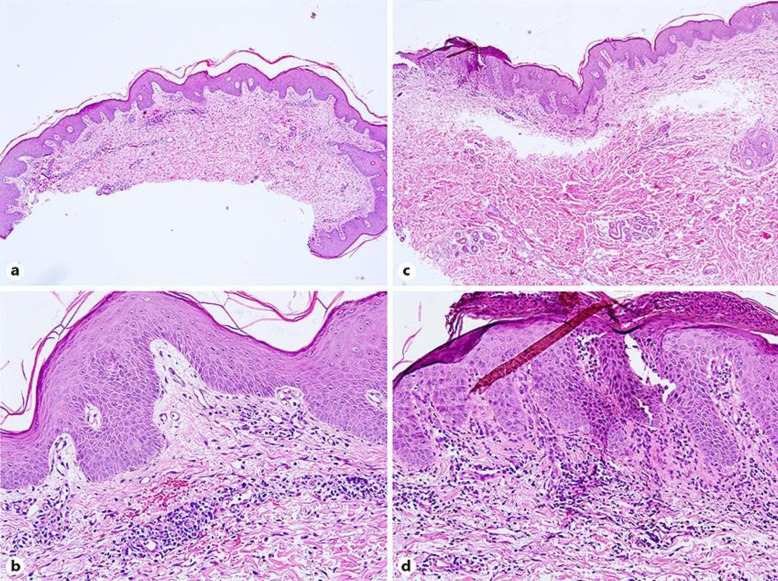
Parakeratosis and minimal hyperplasia in an area of the epidermis. a, b Dermis perivascular infiltrate contained lymphocytes and plasma cells 6 days after admission. a ×40. b ×200. c, d Parakeratosis and intraepidermal neutrophilic granulocyte abscess in an area of the epidermis. Telangiectasia in the dermis papilla, dermal superficial perivascular lymphocytes, and neutrophils infiltration 12 days after admission. c ×40. d ×200.
Presumptive diagnoses of syphilis and AGEP/GPP overlap were both made. The patient was treated with acitretin (20 mg/day) after his admission. Three weeks after admission, the pustular lesions had completely healed (Fig. (Fig.3)3) and the TRUST titer had decreased to 1: 8.

The pustular lesions had healed on the trunk and extremities 3 weeks after admission.
References
1. Sidoroff A, Halevy S, Bavinck JN, Vaillant L, Roujeau JC. Acute generalized exanthematous pustulosis (AGEP) – a clinical reaction pattern. J Cutan Pathol. 2001;28:113–119. [PubMed] [Google Scholar]2. Burrows NP, Russell Jones RR. Pustular drug eruption: a histopathological spectrum. Histopathology. 1993;22:569–573. [PubMed] [Google Scholar]3. Teraki Y, Tanaka S, Hitomi K, Izaki S. A case of generalized psoriasiform and pustular eruption induced by infliximab: evidence for skin-homing Th17 in the pathogenesis. Br J Dermatol. 2010;163:1347–1351. [PubMed] [Google Scholar]4. Onoufriadis A, Simpson MA, Pink AE, Meglio PD, Smith CH, Pullabhatla V, Knight J, Spain SL, Nestle FO, Burden AD, Capon F, Trembath RC, Barker JN. Mutations in IL36RN/IL1F5 are associated with the severe episodic inflammatory skin disease known as generalized pustular psoriasis. Am J Hum Genet. 2011;89:432–437. [PMC free article] [PubMed] [Google Scholar]5. Martins GA, Arruda L. Systemic treatment of psoriasis. Part I. Methotrexate and acitretin. An Bras Dermatol. 2004;79:263–278. [Google Scholar]6. Umezawa Y, Ozawa A, Kawasima T, Shimizu H, Terui T, Taqami H, Ikeda S, Oqawa H, Kawada A, Tezuka T, Iqarashi A, Harada S. Therapeutic guidelines for the treatment of generalized pustular psoriasis (GPP) based on a proposed classification of disease severity. Arch Dermatol Res. 2003;295((suppl 1)):43–54. [PubMed] [Google Scholar]7. Choon SE, Lai NM, Mohammad NA, Nanu NM, Tey KE, Chew SF. Clinical profile, morbidity, and outcome of adult-onset generalized pustular psoriasis: analysis of 102 cases seen in a tertiary hospital in Johor, Malaysia. Int J Dermatol. 2014;53:676–684. [PubMed] [Google Scholar]8. Navarini AA, Valeyrie-Allanore L, Setta-Kaffetzi N, Barker JN, Capon F, Creamer D, Roujeau J-C, Sekula P, Simpson MA, Trembath RC, Mockenhaoupt M, Smith CH. Generalized pustular eruptions: time to adapt the disease taxonomy to the genetic architecture? J Invest Dermatol. 2014;134:580–581. [PubMed] [Google Scholar]9. Navarini AA, Simpson MA, Borradori L, Yawalkar N, Schlapbach C. Homozygous missense mutation in IL36RN in generalized pustular dermatosis with intraoral involvement compatible with both AGEP and generalized pustular psoriasis. JAMA Dermatol. 2015;151:452–453. [PubMed] [Google Scholar]10. Gagari E, Stephanaki C, Rozakou A, Stauropoulos P, Perogianni K, Hadjivassiliou M. Atypical presentation of secondary syphilis in a psoriatic HIV patient. Int J STD AIDS. 2009;20:291–292. [PubMed] [Google Scholar]11. Mikhail GR, Chapel TA. Follicular papulopustular syphilid. Arch Dermatol. 1969;100:471–473. [PubMed] [Google Scholar]12. Waldman GD, Wise RD. Miliary pustular syphilid. Cutis. 1984;34:556–558. [PubMed] [Google Scholar]
Articles from Case Reports in Dermatology are provided here courtesy of Karger Publishers
Department of Dermatology, Shanghai Skin Disease Hospital, Shanghai, China*Yangfeng Ding, Department of Dermatology, Shanghai Skin Disease Hospital, 1278 Baode Road, Jingan District, Shanghai 200000 (China), E-Mail moc.qq@174505529
Copyright © 2018 by S. Karger AG, BaselThis article is licensed under the Creative Commons Attribution-NonCommercial-4.0 International License (CC BY-NC) (http://www.karger.com/Services/OpenAccessLicense). Usage and distribution for commercial purposes requires written permission.