Kerion and tinea capitis
Hidenori Nakagawa,a,⁎ Masato Nishihara,a and Takashi Nakamurab
A 9-year-old boy (Patient 1) with no past medical history presented to the pediatric emergency department with a 1-month history of tender erythematous lesions on his scalp. The lesions had gradually enlarged despite the use of topical antibacterials and corticosteroids. His temperature upon presentation was 38.0℃, and physical examination showed multiple erythematous lesions and tender swellings on his scalp with bilateral cervical lymphadenopathy (Fig. 1). There were no other remarkable signs on examination. Laboratory evaluation showed evidence of an elevated inflammatory response signified by a white blood cell count of 22,800 /μL (84% neutrophils) and a C-reactive protein (CRP) level of 10.99 mg/dL. There were no other apparent abnormalities.
Around the same time, his friend (Patient 2) developed a milder scalp lesion with alopecia. Patient 1 frequently played with cats at Patient 2′s house. Potassium hydroxide wet mount examination of their hair roots showed kinky hyphae and small spores (Fig. 2). Microsporum canis was obtained on culturing Patient 2′s hair specimen. The patients were both treated with oral itraconazole and their lesions gradually improved after a 6-week treatment course. Gradually, the hair of Patient 1 grew back (Fig. 3, Fig. 4).
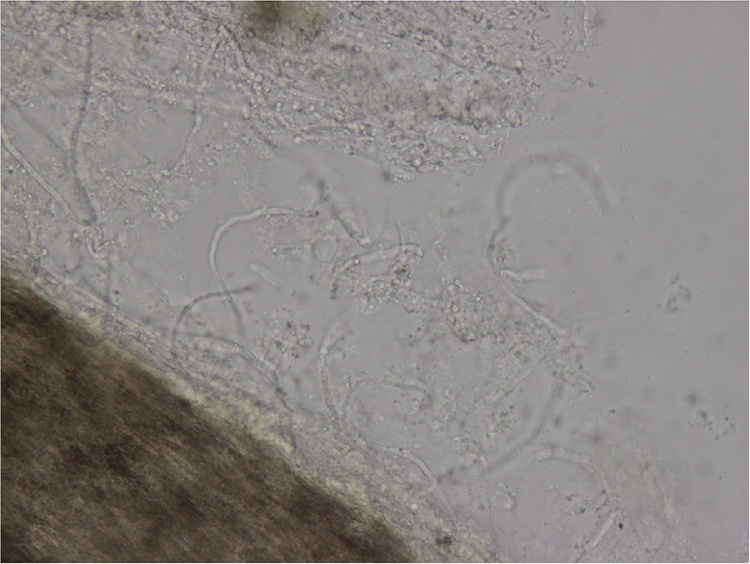
Potassium hydroxide wet mount examination of Patient 1′s hair roots.

The scalp of Patient 1, 1 month after treatment.

The hair of Patient 1 grew back 4 month after treatment.
Tinea capitis is an infection of the scalp hair caused by dermatophyte fungi such as Trichophyton spp. and Microsporum spp. [1]. Kerion is a severe inflammatory form of tinea capitis with a hypersensitivity reaction against dermatophytes [2]. Systemic antifungal therapy is needed for treatment (griseofulvin, terbinafine, fluconazole or itraconazole are the treatments of choice) [3]. The efficacy of adjunctive oral corticosteroids is limited, and thus they are not recommended [4]. The differential diagnosis includes seborrheic dermatitis, bacterial cellulitis, and tumor, and the diagnosis of tinea capitis and kerion is often delayed [5].
References
References
- Hay R.J. Tinea capitis: current status. Mycopathologia. 2017;182:87–93. [PMC free article] [PubMed] [Google Scholar]
- John A.M., Schwartz R.A., Janniger C.K. The kerion: an angry tinea capitis. Int J Dermatol. 2016;57:3–9. [PubMed] [Google Scholar]
- Chen X., Jiang X., Yang M., Gonzalez U., Lin X., Hua X. Systemic antifungal therapy for tinea capitis in children. Cochrane Database Syst Rev. 2016;5:CD004685. [PubMed] [Google Scholar]
- Hussain I., Muzaffar F., Rashid T., Ahmad J., Jahangir M., Haroon T.S. A randomized, comparative trial of treatment of kerion celsi with griseofulvin plus oral prednisolone vs. griseofulvin alone. Med Mycol. 1999;37:97–99. [PubMed] [Google Scholar]
- Feetham J.E., Sargant N. Kerion celsi: a misdiagnosed scalp infection. Arch Dis Child. 2016;101:503. [PubMed] [Google Scholar]
Author information
aDepartment of Pediatrics, Yodogawa Christian Hospital, 1-7-50 Kunijima, Higashiyodogawa-ku, Osaka-shi, Osaka, 533-0024, JapanbDepartment of Dermatology, Yodogawa Christian Hospital, 1-7-50 Kunijima, Higashiyodogawa-ku, Osaka-Shi, Osaka, 533-0024 Japan
Copyright and license information
Copyright © 2018 The Authors
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
