Lower Lip and Chin Reconstruction with Functional Myocutaneous Gracilis Flap
Case Report:
A 50-year-old man presented to the emergency room with a wide lower lip injury caused by a human bite that occurred 2 hours earlier, with avulsion of approximately 80% of the lip and 30% of the chin ( Fig. 1 ). The patient carried the avulsed tissue in an ice bag. Neither history of smoking nor comorbidity was reported.

Preoperative view of the defect.
Surgical Procedure
An emergency surgery was planned to perform a debridement of nonvital tissues and quantify the damage. They attempted a replantation of the avulsed tissue with microsurgical anastomosis of inferior labial vessels ( Fig. 2 ). However, after 3 to 4 hours of good revascularization, an arterial microthrombosis occurred and the replanted tissue was removed.

Replantation of the avulsed lip. Click to unblur
After 3 days, they planned a reconstruction with myocutaneous gracilis flap. The gracilis flap was harvested with an oval-shaped skin paddle of 7 × 5 cm centralized at the longitudinally oriented vessel pedicle (proximal one-third) compared with the muscle fibers ( Figs. 3.4 ).

Flap design. Click to unblur

Gracilis flap with the patient’s overlying skin paddle. Click to unblur
Anastomosis of the vascular pedicle was performed with the facial vessels. While tailoring the flap, they have been careful to give the right tension to the muscle fibers ( Fig. 5 ). Neural anastomosis was also performed between the obturator nerve and the nerve stump of the marginal mandibular nerve. The muscular layer of the flap was shaped for reconstruction of the inner part of the lip, whereas the skin paddle was outward placed. The patient was discharged 8 days after surgery.

Shaping of the flap. Click to unblur
Results and Follow-Up
At 1-month follow-up, the patient was able to open the mouth, laugh, and contain solid foods. After 6 months, the patient showed improvements in daily activities such as fluid containment, complete mouth closure, speaking, blowing, and whistling; complete mucosal metaplasia of the inner layer was observed.
An electromyography was performed after 9 months: muscle activity was predominantly observed in the central part of the flap, with movements such as smiling, whistling, blowing, and lowering the lip. Concerning sensibility, the patient was able to identify deep pressure, and hot-and-cold discrimination test was positive. At 1-year follow-up, good thickness and quality of the skin paddle was observed, and hair transplantation could be now planned ( Fig. 6 ).
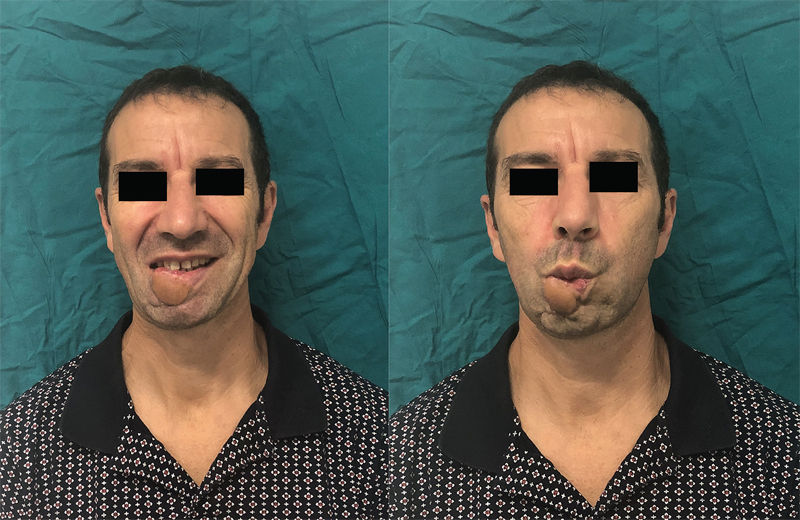
One-year follow-up: patient smiling and blowing.