Scalp burn that occurred during hair coloring
Abstract
Full-thickness scalp burns secondary to hair coloring are rare; however, such defects can be large and complex reconstruction of hair-bearing tissue may be necessary. Many skin-stretching devices that use gradual traction have been applied to take advantage of the viscoelastic properties of the skin. A 21-year-old female patient was seen with a burn defect on her occipital scalp leading to exposed subcutaneous tissue after chemical application of hair coloring in a salon. The dimensions of the wound were 10 cm×5 cm, and a skin graft or flap would have been necessary to close the defect. Two long transfixing K-wires (1.4 mm) and paired 3-wire threads (23 gauge), which are readily available in most hospitals, were applied over a period of 12 days for trichophytic closure of the defect. The remaining scalp scars after primary trichophytic closure with this skin-stretching method were refined with hair follicle transplantation. This skin-stretching method is simple to apply and valuable for helping to close problematic areas of skin shortage that would otherwise require more complicated procedures. This case shows a relatively unknown complication of hair coloring and its treatment.
INTRODUCTION
Persulfates and hydrogen peroxide are the active ingredients in the highlighting mixture used for hair coloring. Commercially available preparations have a much higher concentration of sulfates (up to 60%). Off-the scalp preparations generally have a concentration of approximately 25%. Coagulative necrosis results from direct contact of oxidizing salts with tissues. Hydrogen peroxide is also a powerful oxidizing agent. At the concentration of 10% that is found in many hair coloring materials, it is highly irritating and corrosive, and it can therefore lead to skin blisters and burns.The first skin-stretching device (Sure-Closure) was designed by Hirshowitz et al. Many devices and techniques have been introduced for skin stretching and secure wound closure. However, they were expensive to prepare. The author’s technique is a new and simple method to help close problematic areas of skin shortage that would otherwise require more complicated procedures.
CASE
A 21-year-old female patient was seen with a burn defect on her occipital scalp leading to exposed subcutaneous tissue after chemical application during hair coloring in a salon. Microbiological examination of a swab obtained from the area of ulceration detected moderately high levels of Pseudomonas aeruginosa. Ciprofloxacin was intravenously injected as an antibiotic to which Pseudomonas aureus is sensitive, and Exsalt T7 (Exciton Technologies Inc., Edmonton, AB, Canada) was used for wound dressing. The dimensions of the wound were 10 cm×5 cm, and a skin graft or flap would have been required to close the defect (Fig. 1A).

(A) Full-thickness scalp wound measuring 10 cm×5 cm in the occipital area. (B) Two long transfixed K-wires (1.6 mm) were inserted 2 cm from the wound margins along the long axis of the wound defect. (C) Paired 3-wire threads (23 gauge) bound with K-wires were inserted at the wound border through the subcutaneous layer. (D) Stretching to approximate the wound edges was started by twisting the paired wire threads on both sides after binding the K-wires along the transverse axis of the wound defect. (E) Complete trichophytic closure was achieved by simple interrupted sutures. (F) This patient experienced partial scar widening 2 years after surgery.
The skin-stretching method was applied, and incremental stretching was performed over a period of 12 days until the defect was closed. This method consists of inserting 2-long transfixing K-wires (1.6 mm) 2 cm from the wound margins along the long axis of the wound defect and inserting paired 3-wire threads (23 gauge) at the wound border through the subcutaneous layer after binding the K-wires along the transverse axis of the wound defect (Fig. 1B and C). Stretching for approximation of the wound edges was started by twisting the paired wire threads on both sides. The twisting of the paired wire threads was continued until the patient felt discomfort or blanching or shininess was found at the wound edges. This procedure was repeated until wound margins were approximated so they could be sutured together (Fig. 1D). When this skin-stretching device was used, the upper part of the wound was expected to undergo epithelization, but it gradually deteriorated as the hairs were removed and the tissue damage progressed to granulation tissue. Subsequently, complete trichophytic closure was achieved by simple interrupted suturing with 4/0 Vicryl dermal sutures and 4/0 Mersilk skin sutures (Fig. 1E).The patient experienced partial scar widening 2 years after surgery (Fig. 1F). Therefore, hair follicle transplantation into the scar tissue for aesthetic improvements was performed through the follicular unit extraction method with harvesting from the adjacent occipital scalp (Fig. 2).
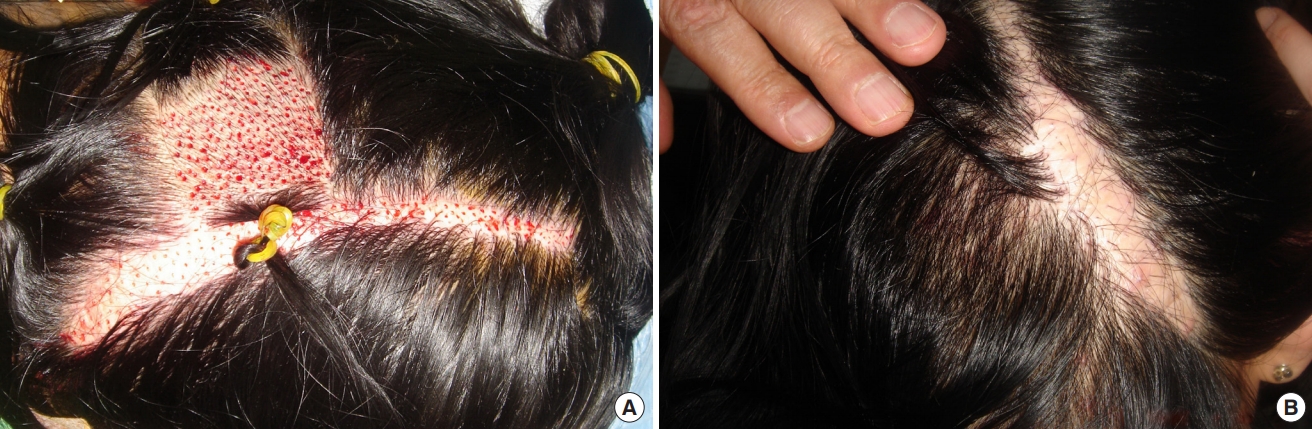
Hair follicle transplantation in the scalp scar
(A) Hair follicle transplantation into the scar tissue for aesthetic improvements was performed by the follicular unit extraction method with harvesting from the adjacent occipital scalp. (B) The donor site of follicular unit extraction and living grafted hairs at 2 months after surgery.