Self-amputation of the Upper Extremity
Erik Marques,1Eric J Maiorino,1Zachary Tallackson,1 and Hossein Masoomi1
Case report
A 28-year-old right-hand dominant male with a history of untreated depression and recent suicidal ideation presented with a complete amputation of the left upper extremity (forearm-level) as the result of an intentional, self-inflicted injury with a circular saw following an argument with his wife (Figure 1). The trauma occurred 45 minutes prior to arrival at our Level I trauma center with the amputated limb appropriately protected and cooled on an ice slurry. The amputation was noted to be a relatively sharp injury at the distal-third forearm-level (Figure 2). Despite a relatively flat affect, the patient appeared to recognize the gravity of the situation, seemed remorseful for his impulsive action, and desired an attempt at replantation. Emergency psychiatry consultation was not obtained because the in-house evaluation was not immediately available, and we did not want to delay operative intervention.

Forearm X-rays demonstrating a transverse radius and ulna forearm fracture at the mid-forearm location. X-rays demonstrate little comminution at the fracture sites.
The patient underwent emergent replantation of the left upper extremity. Bony stabilization was obtained using plate and screw fixation (Figure 3). The radius and ulna were shortened by 4 cm to facilitate primary tension-free repairs of all neurovascular and tendinous structures (Figure 4). Arterial inflow was restored with ulnar artery repair and venous outflow was accomplished with anastomosis of an ulnar artery vena comitans, radial artery vena comitans, and the cephalic vein. The median nerve, ulnar nerve and superficial branch of the radial nerve were repaired primarily. All of the flexor and extensor tendons were repaired using modified Kessler four-strand core sutures. Total ischemia time was not recorded however a tourniquet was used for four hours and 28 minutes, while the arm was prepared for replantation and was let down after bony stabilization. Prophylactic hand fasciotomies were performed. Postoperatively, the patient was monitored on the microsurgery unit and psychiatry consultation was obtained. He was diagnosed with depression without psychosis. Recommendations included mood-stabilizing medication (paroxetine), one-to-one monitoring, and transfer to an inpatient psychiatric facility when cleared by the Plastic Surgery service.
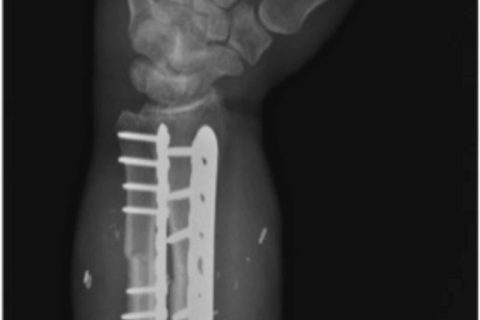
Oblique X-rays demonstrating the radius and ulna forearm fixation after compression plating. Radius and ulna were both shortened by approximately 4 cm to allow for a tension-free repair of the vital soft tissues.
On postoperative day six, the patient was returned to the operating room for closure of the hand fasciotomy wounds and split thickness skin grafting of residual forearm wounds. Hand therapy was initiated after confirmation of good skin graft take and was continued throughout the hospitalization. The patient’s depressed mood stabilized, and he demonstrated a good understanding and commitment to his hand therapy regimen while in-house. Length of hospitalization was 19 days prior to discharge to an inpatient psychiatric facility. The patient continued with hand therapy over the next several months. While all joints remained supple, he developed flexor and extensor tendon adhesions, and later underwent flexor and extensor tenolysis at six months after replantation.
At six years postoperatively, the patient was extremely satisfied with the function and appearance of the replanted extremity (despite the development of hypertrophic scarring) (Figure 5). He demonstrated good composite flexion and extension, sensory recovery of 7-9 mm two-point discrimination to all fingers and thumb and incomplete recovery of intrinsic function with functional thumb opposition (Figure 6). He has returned to his previous employment as a laboratory technician without restrictions. Dash score was 5.8 with a Chen Grade I (excellent) functional recovery (Figure 7). From a psychiatric standpoint, he was continued on paroxetine with improvement in his depressive symptoms.

Image depicting the palmar aspect of the hand and forearm six years postoperative, demonstrating the moderate hypertrophic scarring from the patient’s previous procedures. These scars did not affect his overall functional outcome.

Postoperative functional outcomePatient demonstrating prehensile function of the replanted hand

Postoperative fine motor outcome
Patient demonstrating hook grasp and pinch function
Keywords: self-amputation, acute psychosis, replantations
Copyright © 2019, Marques et al.

