Squamous cell carcinoma in a child with xeroderma pigmentosum: Clinical response with photon beam radiation therapy
A 7-year-old male pupil presented to the radiotherapy outpatient department of our hospital with raised, everted, and ulcerated ulcer on the anterior tongue with associated oral fetor. There were associated progressive difficulty in swallowing, poor vision, and generalized scaly pigmented skin which the parents noticed about 11 months prior. There were multiple bleeding and pus-discharging masses in the parieto-occipital and frontal regions of the scalp which first appeared about 9 months before presentation and became more florid over the last 3 months.
The patient was a child of a termed uneventful pregnancy to nonconsanguineous parents. He had seven other siblings. He reportedly lost the four earlier siblings (a girl and three boys) to a condition with similar presentation; all died before reaching the age of 4 years (age at death was 29 months, 47 months, and 39 months, respectively). The remaining three siblings (a girl and 2 boys aged 16, 11, and 9 years, respectively) are alive and well without any symptoms related to XP. Both parents were unaffected by this condition and are of low socioeconomic background.
Symptoms date back to his third birthday when the mother noticed few skin changes including freckling on the face and upper limbs, hyper-pigmented and hypo-pigmented lesions on the face, and difficulty in seeing which progressed to complete blindness in the left eye at 4 years. He developed a nonhealing ulcer on the left antero-lateral aspect of the tongue at about age of six.
Physical examination revealed a small-for-age boy, with evidence of malnutrition, blind in the left eye, and had multiple inverted cone-like sharply demarcated lesions on the scalp. Some of the scalp lesions were oozing purulent discharges. The largest lesion measured 2 cm by 3 cm and the smallest 0.5 cm by 1 cm. The scalp was also covered with multiple scaly plaques, which were more pronounced on the fronto-parietal region. Most of his sun-exposed skin areas, especially the scalp, face, neck, and upper trunk were dry and scaly and had a mixture of mottled, hyper-pigmented, and hypo-pigmented lesions. These lesions were less obvious on the lower limbs and appeared atrophic with few areas of telangiectasia at the right fronto-parietal region.
The skin over the flexure surfaces of the wrist and elbows, bilaterally, appeared thickened. Both corneas were cloudy with loss of light perception in the left eye. An intra-oral examination was remarkable for a fungating papillomatous mass measuring 2 cm by 2 cm along the left lateral border of the anterior tongue, which appeared hemorrhagic and apparently infected. There is an associated oral fetor due to very poor oral hygiene with leukoplakia and cheilitis. There were no palpable cervical lymph nodes. There was no obvious neurological abnormality and other systems were normal. Blood investigations revealed a picture of reduced mean corpuscular volume, low mean corpuscular hemoglobin, hypochromia, and microcytosis which are consistent with findings in chronic anemia. The packed cell volume was 24%. Erythrocyte sedimentation rate, lipid profile, liver function, renal function, serum electrolytes tests, and urinalysis were all normal. Plain chest X-ray, ultrasonography of the abdomen and pelvis, and electrocardiography were within normal limits. Ophthalmic examination revealed bilateral conjunctivitis, dry eyes, cornea scarring, blepharitis, and bilateral cataracts.
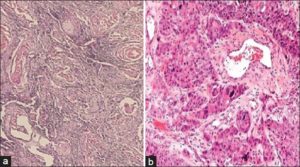
Incisional biopsies of the scalp lesions and the tongue tumor were done. Histopathological examination of the biopsied specimens revealed well-differentiated SCC [Figure 2]. On the basis of the characteristic cutaneous and ocular lesions associated with sunshine hypersensitivity and histologically proven SCC of both tongue and scalp lesions, a diagnosis of XP in its final phase (phase three), the cancerous period was made.
The patient was transfused with blood to correct for anemia and treated with broad spectrum antibiotics (clavulanate potentiated amoxicillin and metronidazole) to control apparent scalp and intraoral infections. Because of imminent severe hemorrhage from the tongue tumor, he was planned for palliative external beam radiotherapy. Radiation dose of 45 Gy given in 25 fractions over a period of 5 weeks was administered to the anterior tongue using a left face orthogonal fields, and a further dose of 15 Gy given in five fractions over 5 days to ulcerated/bleeding scalp lesions by direct portal. The patient tolerated the radiation treatment well. The malignant tumors responded excellently to treatment with control of bleeding from the scalp, and the tongue lesion completely resolved within 9 weeks with improvement in feeding [Figure 3] and [Figure 4]. The patient had done well in the posttreatment period with no new tumor lesions arising from radiotherapy treated areas but was, however, lost to follow-up after 12 months.

Figure 4: Good local control of the anterior-lateral tongue squamous cell carcinoma lesion after palliative external beam radiotherapy. Note, facial skin freckles and areas of hyper- and hypo-pigmentation

