Trajectory of Cardiac Catheterization for Acute Coronary Syndrome and Out-of-Hospital Cardiac Arrest During the COVID-19 Pandemic
Background
We sought to investigate the trajectory of cardiac catheterizations for acute coronary syndrome (ACS) and out-of-hospital cardiac arrest (OHCA) during the pre-isolation (PI), strict-isolation (SI), and relaxed-isolation (RI) periods of the coronavirus disease 2019 (COVID-19) pandemic at three hospitals in Los Angeles, CA, USA.
Methods
A retrospective analysis was conducted on adult patients undergoing urgent or emergent cardiac catheterization for suspected ACS or OHCA between January 1, 2020 and June 2, 2020 at three hospitals in Los Angeles, CA, USA. We designated January 1, 2020 to March 17, 2020 as the PI COVID-19 period, March 18, 2020 to May 5, 2020 as the SI COVID-19 period, and May 6, 2020 to June 2, 2020 as the RI COVID-19 period.
Results
From PI to SI, there was a significant reduction in mean weekly cases of catheterizations for non-ST elevation myocardial infarction/unstable angina (NSTEMI/UA) (8.29 vs. 12.5, P = 0.019), with all other clinical categories trending downwards. From SI to RI, mean weekly cases of catheterizations for total ACS increased by 17%, NSTEMI/UA increased by 27%, and OHCA increased by 32%, demonstrating a “rebound effect”.
Conclusions
Cardiac catheterizations for ACS and NSTEMI/UA exhibited a “rebound effect” once social isolation was relaxed.
Introduction
Recent studies demonstrated a worrisome decline in cardiac catheterizations for acute coronary syndrome (ACS) during the initial peak of the coronavirus disease 2019 (COVID-19) pandemic. Once the incidence of new COVID-19 cases appeared to decrease, isolation orders were relaxed across the country. We sought to investigate if this relaxed-isolation (RI) period was associated with an increase in cardiac catheterizations for ACS and out-of-hospital cardiac arrest (OHCA) requiring catheterization lab activation, thereby demonstrating a “rebound effect” following the first peak of COVID-19.
Materials and Methods
We performed a retrospective analysis of adult patients undergoing urgent or emergent cardiac catheterization for suspected ACS or OHCA between January 1, 2020 and June 2, 2020 at three hospitals in Los Angeles, CA, USA. We designated January 1, 2020 to March 17, 2020 as the pre-isolation (PI) COVID-19 period, March 18, 2020 to May 5, 2020 as the strict-isolation (SI) COVID-19 period, and May 6, 2020 to June 2, 2020 as the RI COVID-19 period. The Institutional Review Board of University of California, Los Angeles, approved this study and waived patient consent given the retrospective nature of the study. This study was conducted in compliance with all the applicable institutional ethical guidelines for the care, welfare and use of animals.
We included all adult (age ≥ 18 years) patients with cardiac catheterizations for ACS, ST-elevation myocardial infarction (STEMI) activations, true STEMI, non-STEMI/unstable angina (NSTEMI/UA), and OHCA. STEMI activation was defined as a catheterization lab activation for a presumed STEMI or OHCA. ACS was defined as true STEMI or NSTEMI/UA. True STEMI was defined by the presence of a culprit lesion on angiogram. For all cases, we collected baseline demographic and cardiovascular risk factor data.
We compared cardiac catheterization volume for each clinical category (ACS, STEMI activation, true STEMI, NSTEMI/UA, OHCA) for each time period. One-way analysis of variance (ANOVA) or Fisher’s exact tests were used to evaluate differences between groups of variables, as appropriate. We performed one-way ANOVA to evaluate if cases per week of ACS, STEMI activation, STEMI, NSTEMI/UA, and OHCA differed across PI, SI, and RI. Post hoc analysis was completed using Tukey’s test. All statistical analyses were completed using STATA 16.1 MP (College Station, TX, USA), and a P value < 0.05 was considered statistically significant.
Results
Overall, 377 patients were included in this study, with 211 patients during PI, 99 patients during SI, and 67 patients during RI. Baseline demographic and clinical characteristics were similar among the three groups (Table 1). There was a statistically significant difference in cardiac catheterization cases for NSTEMI/UA between groups (P = 0.025 for interaction (ANOVA)). This was driven by a significant difference in the mean number of cases per week of NSTEMI/UA in SI relative to PI (8.29 vs. 12.5, P = 0.019). There were no statistically significant differences in the other clinical scenarios (ACS, STEMI activation, OHCA) in SI relative to PI. However, trends toward an increase in cases in RI relative to SI were observed in ACS, NSTEMI/UA, and OHCA. Specifically, from SI to RI, the mean weekly number of catheterization cases for ACS increased by 17%, NSTEMI/UA increased by 27%, and OHCA increased by 32% (Fig. 1).
Table 1
Demographics and Clinical Characteristics of Patients Undergoing Urgent or Emergent Cardiac Catheterization for Each Clinical Scenario in the Time Period Pre-Isolation (January 1, 2020 to March 17, 2020), Strict-Isolation (March 18, 2020 to May 5, 2020), and Relaxed-Isolation (May 6, 2020 to June 2, 2020)
| All | Pre-isolation (n = 211) | Strict-isolation (n = 99) | Relaxed-isolation (n = 67) | P value | |
|---|---|---|---|---|---|
| Male | 74% | 72% | 74% | 77% | 0.75 |
| Age (years) | 65.4 | 65.0 ± 13.7 | 65.0 ± 12.0 | 67.4 ± 11.7 | 0.41 |
| Prior coronary artery disease | 41% | 40% | 39% | 44% | 0.77 |
| Hyperlipidemia | 59% | 53% | 63% | 67% | 0.07 |
| Hypertension | 71% | 67% | 71% | 79% | 0.21 |
| Diabetes mellitus | 38% | 40% | 34% | 37% | 0.55 |
| Chronic kidney disease | 22% | 19% | 27% | 20% | 0.29 |
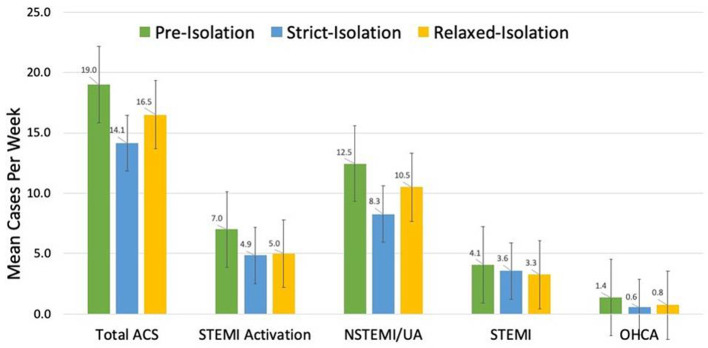
Mean number of cases per week for each clinical scenario during the time periods pre-isolation (January 1, 2020 to March 17, 2020), strict-isolation (March 18, 2020 to May 5, 2020), and relaxed-isolation (May 6, 2020 to June 2, 2020). Standard error bars are shown. *Statistically significant difference with a P value < 0.05. ACS: acute coronary syndrome; NSTEMI: non-ST elevation myocardial infarction/unstable angina; UA: unstable angina; OHCA: out-of-hospital cardiac arrest.
Author information
aDepartment of Internal Medicine, UCLA Medical Center, Los Angeles, CA, USA
bDivision of Interventional Cardiology, UCLA Medical Center, Los Angeles, CA, USA
cDivision of Congenital Cardiology, UCLA Medical Center, Los Angeles, CA, USA
dUCLA Cardiology Group, Henry Mayo Hospital, Valencia, CA, USA
eCorresponding Author: Pooja S. Desai, Department of Internal Medicine, UCLA Medical Center, 757 Westwood Avenue, Suite 7501, Los Angeles, CA, USA.