Angioedema, an unusual reaction to hair dye
Reginald Mzudumile Ngwanya,1,&Zandile Spengane,1 and Nonhlanhla Khumalo1
Summary of Drugs used: Hydrocortisone, Phenergan, Vitamin D, Calcium tablets, Chlorpheniramine maleate, Cetomacrogol cream, Clobetasol, Methylprednisolone
Introduction
Paraphenynlenediamine (PPD) a potent skin sensitizer is a cause of allergic contact dermatitis, a type-IV hypersensitivity reaction. It is a constituent of hair dyes and is also added to red henna thereby creating black henna. Skin reactions to PPD include angioedema urticarial and anaphylactic reactions. There are systemic manifestations of PPD poisoning such as acute kidney injury, rhabdomyolysis and toxic myocarditis. Angioedema, a type-1 hypersensitivity reaction, is characterised by swelling of the skin and subcutaneous tissue. In addition to skin it affects respiratory and gastrointestinal systems and presents with laryngeal swelling that can be life threatening. It is important to recognise the condition early so not to give inappropriate treatment.
Patient and observation
A 29 year old lady presented to the Dermatology Department at Groote Schuur Hospital with a 2 day history of severe swelling of her face, marked periorbital oedema which developed overnight. She had used henna hair dye containing paraphenynlenediamine (PPD) the previous day. There was no history of previous sensitization with the use of hair dye or tattoos using black henna. Patient was initially treated at a pharmacy and given Amoxicillin for a presumed diagnosis of cellulitis. She was then later taken to a day hospital in the early morning on Day 2 of symptoms where she received hydrocortisone 200mg intravenously and Phenergan 25mg intramuscularly both as stat doses. This made no improvement and the patient was referred to a tertiary hospital. On arrival at Groote Schuur hospital she was given repeat hydrocortisone 100mg intravenously and Phenergan 25mg intramuscularly. She had severe facial oedema with marked periorbital oedema (Figure 1). There was no swelling of the tongue. She had scale crust on her scalp. Skin punch biopsy was unremarkable. The patient was admitted into our dermatology ward and put on prednisone 40mg orally daily, Vitamin D weekly, calcium tablets and chlorpheniramine maleate 4mg daily. Topically she received cetomacrogol cream to de-crust her scalp. Once de-crusted, clobetasol cream was applied. She also applied clobetasol cream to her face for 4 days which was weaned down to methylprednisolone on day 5 and weaned down to 1% hydrocortisone ointment on day seven. The patient made a full recovery by day 5 and discharged on Cetomacrogol and fluocinolone gel for scalp and 1% hydrocortisone ointment for the face (Figure 2). A standard patch test that was subsequently done showed positive patch test to PPD (Figure 3).
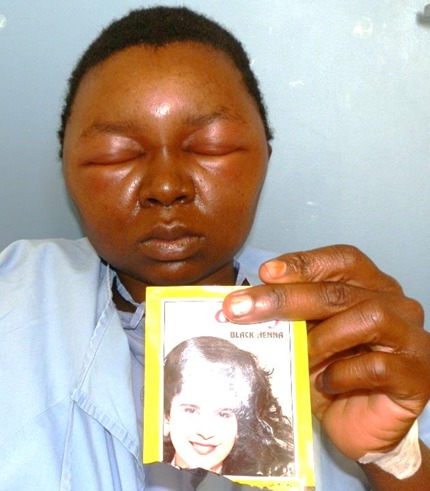
Clinical photograph showing swollen face

Clinical photograph 5 days later

Standard patch test showing a positive reaction to PPD
Conclusion
It is important for the physicians to be aware of the differential diagnosis of a red swollen face that it is not cellulitis only and angioedema-like reactions should be included as these would require a different approach to the management. The learning points in this case highlight the fact that the differential diagnosis of facial swelling must also include contact dermatitis to hair products. Accurate diagnosis is needed for correct and prompt treatment and labelling of black henna should state the presence of PPD and the dangers linked with its use.
Author information
Article notes
Copyright and License information
Disclaimer
References
- Patra AP, et al. Paraphenylenediamine containing hair dye: an Emerging Household Poisoning. Am J Forensic Med Pathol. 2015 Sep;36(3):167–71. [PubMed] [Google Scholar]
- Gokalp H, Kaya K. Angioedema-like allergic contact dermatitis related to black henna. Dermatol Online J. 2014 Feb 18;20(2) [PubMed] [Google Scholar]
- Kind F, Scherer K, Bircher AJ. Contact dermatitis to para-phenylenediamine in hair dye following sensitization to black henna tattoos – an ongoing problem. J Dtsch Dermatol Ges. 2012 Aug;10(8):572–8. [PubMed] [Google Scholar]
- Haluk Akar H, et al. Hair dyes and temporary tattoos are a real hazard for adolescents? Eur Ann Allergy Clin Immunol. 2014 Jan;46(1):35–7. [PubMed] [Google Scholar]
- Matulich J, Sullivan J. A temporary henna tattoo causing hair and clothing dye allergy. Contact Dermatitis. 2005 Jul;53(1):33–6. [PubMed] [Google Scholar]
- Patel S, et al. Patch test frequency to p-phenylenediamine: follow up over the last 6 years. Contact Dermatitis. 2007 Jan;56(1):35–7. [PubMed] [Google Scholar]
- Spornraft-Ragaller P, et al. Severe allergic reactions to para-phenylenediamine in children and adolescents: should the patch test concentration of PPD be changed? J Dtsch Dermatol Ges. 2012 Apr;10(4):258–64. [PubMed] [Google Scholar]
Articles from The Pan African Medical Journal are provided here courtesy of African Field Epidemiology Network