Intraocular eyelashes and iris cyst in anterior chamber following penetrating eye injury: a case report
Sabin Sahu,1 Lila Raj Puri,1 and Sanjay Kumar Singh2
Case report
A 24-year-old Nepalese male presented with decreased vision in the left eye noticed for last 2 weeks. His visual acuity was 6/6 in the right eye and 6/18 in the left eye, improving to 6/9 with −2.5 DC × 140° correction. The intraocular pressure was 12 mmHg in both eyes. On slit-lamp examination, the left eye showed 8 mm linear peripheral corneal opacity nasally. In the anterior chamber, two curvilinear foreign bodies were seen superiorly resembling eyelashes, and an iris cyst measuring 4 mm × 4 mm was seen (Figure 1). The anterior chamber was quiet, and there was no posterior synechia. Gonioscopy examination revealed normal angle structures and no foreign bodies. The pupil appeared slightly oval but was reacting normally to light. Lens was clear, and dilated fundus examination did not reveal any abnormality. The right eye was normal. Ocular history revealed past history of trauma in the left eye with a metallic wire while working in a construction site abroad 2 years back. No medical care was sought at that time. There was no history of past ocular surgeries.
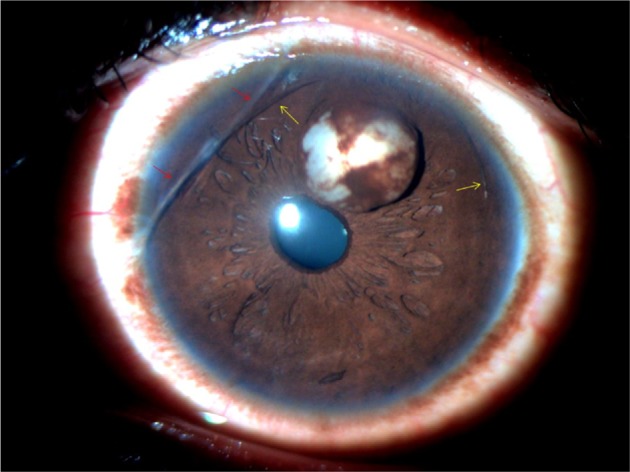
Slit-lamp photograph of the anterior segment at presentation showing iris cyst, two eyelashes in the anterior chamber (yellow arrows) and linear corneal opacity (red arrows).
The eyelashes and the iris cyst were removed surgically. The anterior chamber was entered at the superotemporal limbus, and viscoelastic substance was introduced. The lashes were removed, and the cyst was excised in toto with a sectoral iridectomy. There was no collateral damage to other ocular structures. Postoperatively, there was transient anterior segment inflammation and microscopic hyphema, which subsided with topical antibiotic–steroid combinations. The visual acuity in the left eye eventually improved to 6/6 with −1.5 DC × 130° correction. The patient did not complain of glare despite the broad iridectomy (Figure 2). There were no complications in the 3-month follow-up period.
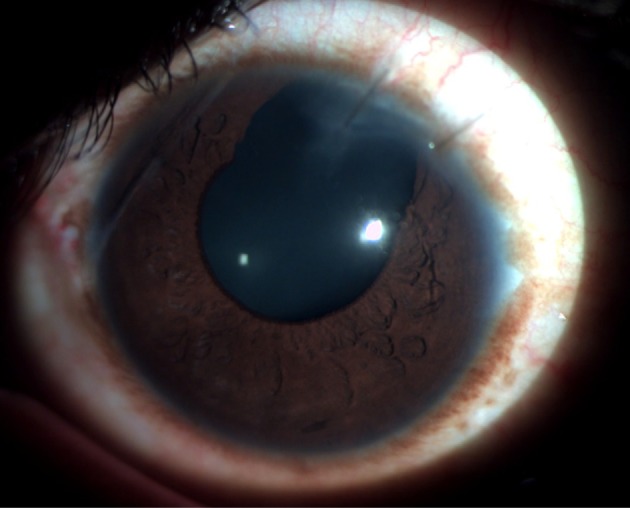
Slit-lamp photograph of the anterior segment 1 week postoperatively showing the sectoral surgical iridectomy.
Discussion
The intraocular eyelashes are usually well tolerated and remain asymptomatic due to their relatively inert nature compared to other organic materials and the immune-privileged feature of the eye.12 The posttraumatic intraocular cilia have been reported to remain silent for 50 years.10 The intraocular eyelashes may be associated with corneal edema, granulomatous inflammation, cyst formation, intralenticular abscess, retinal detachment, endophthalmitis and even sympathetic ophthalmia.3,4,12–14 Various treatment modalities have been described for treatment of iris cyst with varying outcomes. Small and asymptomatic cysts may be closely observed, while the larger cysts require surgical management.15 Conservative surgical approaches such as aspiration of the cyst have been described but are associated with a high rate of recurrence.16 Intracystic injections of low-dose anti-mitotic agents have also been found useful in recurrent secondary iris cyst.17 Needle aspiration and endodiathermy treatment of epithelial inclusion cyst of the iris have also been reported to have a good result.18 Lasers play an important role in the management of iris cysts. Lasers can be used alone or in conjunction with other treatment modalities of the iris cyst. Laser iridotomy of the cyst offers a noninvasive method of therapy for posttraumatic iris inclusion cysts but is associated with a high rate of recurrence.19 Viscoelastic dissection of the posttraumatic iris cyst has been described with an acceptable long-term outcome.20 Viscoelastic-assisted endophotocoagulation has been documented to have an excellent response in the management of secondary iris cysts.21 Various other forms of surgical excision include sector iridectomy, iridectomy plus cryotherapy, iridocyclectomy, iridectomy with corneal curettage and posterior corneal lamellar dissection.22 In our case, sector iridectomy was done to excise the iris cyst in toto along with the intraocular eyelashes removal through the limbal approach. Viscoelastic substance was used so that the cyst could be excised with minimal trauma to the corneal endothelium and adjacent ocular structures. The postoperative visual outcome was good, and there were no significant complications associated with the procedure.
Conclusion
Intraocular implantation of eyelashes following penetrating eye injury can remain asymptomatic for a long period; however, late development of iris cyst may occur. Various surgical techniques, ranging from minimally invasive laser procedures to extensive surgical procedures, have been described with variable outcomes. We report a relatively uncommon case with coexistence of two intraocular eyelashes and a secondary iris cyst after 2 years of asymptomatic period following penetrating eye injury and its successful management with intraocular eyelashes removal and sector iridectomy.
References
- Hoh H, Menage M. Iris cysts after traumatic implantation of an eyelash into the anterior chamber. Br J Ophthalmol. 1993;77(11):741–742. [PMC free article] [PubMed] [Google Scholar]
- Köse S, Kayikçioğlu O, Akkin C, Yağci A, Basdemir G. Coexistence of intraocular eyelashes and anterior chamber cyst after penetrating eye injury: a case presentation. Int Ophthalmol. 1994–1995;18(5):309–311. [PubMed] [Google Scholar]
- Gopal L, Banker AS, Sharma T, Parikh S, Bhende PS, Chopra S. Intra-ocular cilia associated with perforating injury. Indian J Ophthalmol. 2000;48(1):33–36. [PubMed] [Google Scholar]
- Galloway GD, Ang GS, Shenoy R, Beigi B. Retained anterior chamber cilium causing endophthalmitis after phacoemulsification. J Cataract Refract Surg. 2004;30(2):521–522. [PubMed] [Google Scholar]
- Islam N, Dabbagh A. Inert intraocular eyelash foreign body following phacoemulsification cataract surgery. Acta Ophthalmol Scand. 2006;84(3):4324. [PubMed] [Google Scholar]
- Walker NJ, Hann JV, Talbot AW. Postoperative cilium entrapment by clear corneal incision. J Cataract Refract Surg. 2007;33(4):733–734. [PubMed] [Google Scholar]
- Oh KT-(Kean), Oh KT-(Kong), Singerman LJ. An eyelash in the vitreous cavity without apparent etiology. Ophthalmic Surg Lasers. 1996;27(3):243–245. [PubMed] [Google Scholar]
- Kertes PJ, Al-Ghamdi AA, Brownstein S, Coupal D, Gilberg S, Britton WA., Jr An intraocular cilium of uncertain origin. Can J Ophthalmol. 2004;39(3):279–281. [PubMed] [Google Scholar]
- Kargi SH, Oz O, Erdinc E, Teke MY, Firat E. Tolerated cilium in the anterior chamber. Ocul Immunol Inflamm. 2003;11(1):73–78. [PubMed] [Google Scholar]
- YalnizAkkaya Z. Posttraumatic cilia remaining inert in the anterior chamber for 50 years: a case report. J Med Case Rep. 2011;5:527. [PMC free article] [PubMed] [Google Scholar]
- Taneja S, Arora R, Yadava U. Fingernail trauma causing corneal laceration and intraocular cilia. Arch Ophthalmol. 1998;116(4):530–531. [PubMed] [Google Scholar]
- Humayun M, de la Cruz Z, Maguire A, Dangel ME, Stark WJ, Green WR. Intraocular cilia. Report of six cases of 6 weeks’ to 32 years’ duration. Arch Ophthalmol. 1993;111(10):1396–1401. [PubMed] [Google Scholar]
- Gottlieb F, Finestone J, Ackerman JL. Intravitreal cilia and retinal detachment. Ann Ophthalmol. 1982;14(6):541–544. [PubMed] [Google Scholar]
- Dettoraki M, Andreanos K, Davou S, Nomikarios N, Moschos MM, Brouzas D. Intravitreal cilium associated with retinal detachment 40 years following penetrating eye injury: a case report. BMC Ophthalmol. 2015;15:25. [PMC free article] [PubMed] [Google Scholar]
- Haller JA, Stark WJ, Azab A, Thomsen RW, Gottsch JD. Surgical management of anterior chamber epithelial cysts. Am J Ophthalmol. 2003;135(3):309–313. [PubMed] [Google Scholar]
- Shields JA, Shields CL, Lois N, Mercado G. Iris cysts in children: classification, incidence, and management. Br J Ophthalmol. 1999;83(3):334–338. [PMC free article] [PubMed] [Google Scholar]
- Kawaguchi K, Yamamoto S, Nagae Y, et al. Treatment of recurrent giant iris cyst with intracyst administration of mitomycin C. Br J Ophthalmol. 2000;84(7):800–801. [PMC free article] [PubMed] [Google Scholar]
- Tsai JC, Arrindell EL, O’Day DM. Needle aspiration and endodiathermy treatment of epithelial inclusion cyst of the iris. Am J Ophthalmol. 2001;131(2):263–265. [PubMed] [Google Scholar]
- Gupta V, Rao A, Sinha A, Kumar N, Sihota R. Post-traumatic inclusion cysts of the iris: a long term prospective case series. Acta Ophthalmol Scand. 2007;85(8):893–896. [PubMed] [Google Scholar]
- Al-Ghadeer H, Al-Towerki AE, Al-Rajhi A, Al-Awad A. Longterm follow-up and visual outcome after excision of a traumatic iris cyst by viscoelastic dissection. Int Ophthalmol. 2011;31(6):529–531. [PubMed] [Google Scholar]
- Lockington D, Altaie R, Moore S, McGhee CN. Successful management of secondary iris cysts with viscoelastic-assisted endophotocoagulation. JAMA Ophthalmol. 2014;132(3):354–356. [PubMed] [Google Scholar]
- Rao A, Gupta V, Bhadange Y, Sharma R, Shields JA. Iris cysts: a review. Semin Ophthalmol. 2011;26(1):11–22. [PubMed] [Google Scholar]
Articles from International Medical Case Reports Journal are provided here courtesy of Dove Press
Author information
1Department of Ophthalmology, Sagarmatha Choudhary Eye Hospital, Lahan, Siraha
2Department of Ophthalmology, Biratnagar Eye Hospital, Biratnagar, Nepal
Correspondence: Sabin Sahu, Sagarmatha Choudhary Eye Hospital, Lahan-3, Siraha, Nepal, Tel +977 98 6222 3692, Fax +977 33 560 492
Email: sabinsahu@gmail.com
Copyright and License information
Copyright © 2017 Sahu et al. This work is published and licensed by Dove Medical Press Limited
The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed.