Surgical Excision of Madelung Disease Using Bilateral Cervical Lymphnode Dissection Technique—Its Effect and the Influence of Previous Injection Lipolysis
Erika Andou, MD,* Masakazu Komoto, MD,* Toshio Hasegawa, MD,† Hiroshi Mizuno, MD,* and Ayato Hayashi, MD
CASE REPORT
A 51-year-old man was presented to our facility with large subcutaneous tumors affecting the entire neck. Eight years earlier, he was diagnosed with Madelung disease based on the characteristic presentation of symmetrical subcutaneous tender masses throughout the body. Pathological and magnetic resonance imaging (MRI) findings showed that all the masses were lipomatous. The patient had a history of chronic alcohol abuse. At 46 years old, he underwent a shoulder lipectomy and monthly injection lipolysis of the neck for 7 months, which resulted in moderate improvement of the diseases.
Four years later, he experienced sudden deafness and was administered 10 mg betamethasone (intravenous drip tapered over 8 days), followed by 5 mg prednisolone for 10 days. Following steroid administration, progression of the neck lipomatosis was noted, and the patient was unable to fasten his shirt buttons (Fig. 1). When he visited our facility, the circumferences of the mandible and suprasternal notch were 52 cm and 58 cm, respectively.

At initial presentation to our facility: Frontal view (A) and lateral view (B). The subcutaneous tumors over his entire neck had increased in size and he could not fasten his shirt buttons.
He had no history of smoking but had consumed 360 mL/d of sho-chu alcohol (25–35% vol/vol) for the past 20 years.
MRI images showed a high-intensity, clearly marginated, widely dispersed, fat-intense mass in the posterior and bilateral neck that was located beneath the platysma and trapezius muscles (Fig. 2).
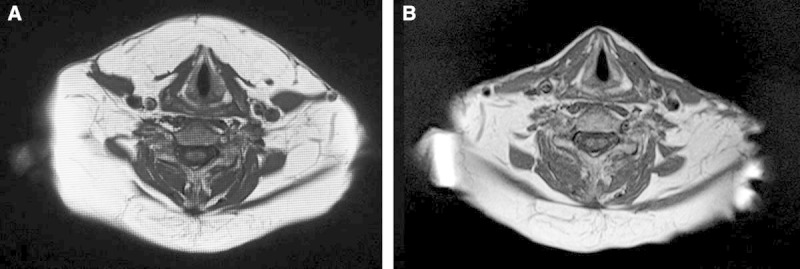
Preoperative and postoperative T1-weighted MRI images. A, Preoperative image. B, Postoperative image 32 months after the surgery. Preoperative image shows a high-intensity, clearly marginated, fat-intense mass in the posterior bilateral neck, which was identified as a lipoma. The mass extends widely beneath the platysma muscle and does not compress the trachea. Postoperative image shows no lipoma masses beneath the platysma.
We planned to perform liposuction to the submental area and radical excision of the mass using the cervical lymph node dissection technique for the lateral and posterior aspects of the neck, where the tumor extended deeply.
An S-line incision was made anterior to the ear, and multiple lipomas were visible beneath the platysma. We attempted to remove the lipomas completely using cervical neck lymph node dissection to prevent recurrence from the residual fat tissue; however, the lipomas were strongly adherent to the surrounding tissues, and gentle manipulation was required to preserve major nerves and vessels.
We then attempted liposuction at the submental area, but suction was hampered because of lipoma fibrosis, and all the masses were eventually dissected (Fig. 3).

Fig. 3.
Intraoperative findings and pathological images. A, Postexcision image. The resected masses weighed 250 g (right posterior) and 240 g (right anterior). B, Histopathological image of the surgical specimens (hematoxylin and eosin stain, ×40). Necrosed adipocytes (arrow) and fibrous tissue (arrowheads) were likely caused by the previous injection lipolysis.
The excised lipomas weighed 250 g (bilateral submental area), 240 g (right posterior neck), and 130 g (left posterior neck) (Fig. 3).
On histopathological examination, the majority of lipomas were composed of variable-sized adipocytes; others were composed of necrotic adipocytes and fibrous tissues that may have developed as a result of previous injection lipolysis (Fig. 3).
The patient did not experience any postoperative complications such as hematoma or seroma, and he was discharged from the hospital on the 10th postoperative day.
At 1 year postoperatively, the circumferences of the mandible and suprasternal notch had decreased to 39 cm and 43 cm, respectively. The patient complained of desensitization to the side of the neck, which persisted but was slowly recovering.
At the 32nd postoperative month, despite our recommendation to abstain from alcohol consumption, the patient continued to drink. However, he had good cosmetic results, with no recurrence of the cervical lipomatosis, and he was able to fasten his shirt buttons (Fig. 4). An MRI 32 months postoperatively showed no recurrence of the lipomatosis beneath the platysma or trapezius muscles (Fig. 2).
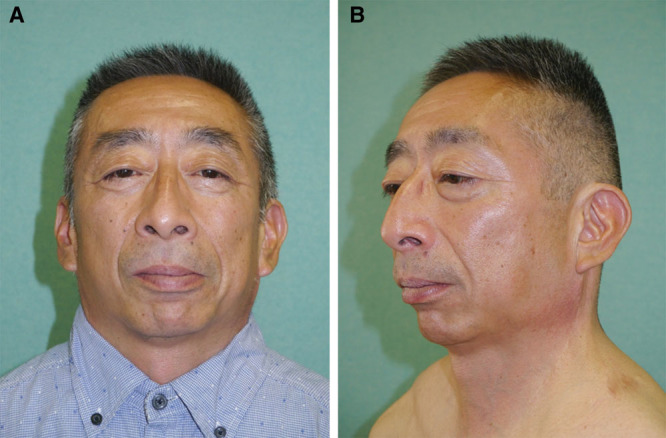
At 26 postoperative months: Frontal view (A) and lateral view (B). The patient shows good cosmetic results, with no recurrence of the cervical lipomatosis.
Author information
From the *Department of Plastic and Reconstructive Surgery, Juntendo University School of Medicine, Tokyo, Japan; and †Department of Dermatology, Juntendo University School of Medicine, Tokyo, Japan.
corresponding authorCorresponding author.
Ayato Hayashi, MD, Department of Plastic and Reconstructive Surgery, Juntendo University School of Medicine, 2-1-1 Hongo Bunkyo-ku, Tokyo 113–8421, Japan, E-mail: ayhayasi@juntendo.ac.jp
References
REFERENCES
- Brodie BC. Clinical Lectures on Surgery: Delivered at St George’s Hospital. Philadelphia: Lea & Blanchard; 1864. pp. 201–202. [Google Scholar]
- Madelung OW. Ueber der Fetthals (diffuses Lipom des Halses). Arch-Klin-Chir. 1888;37:106–130. (in German) [Google Scholar]
- Hasegawa T, Matsukura T, Ikeda S. Mesotherapy for benign symmetric lipomatosis. Aesthetic Plast Surg. 2010;34:153–156. [PubMed] [Google Scholar]
- Kuroda M, Sakamaki M. A case of Madelung disease progressed because of alcohol abuse after first surgery. J Jpn Soc Intern Med. 2010;30:72–76. (in Japanese) [Google Scholar]
- Mikawa K, Nishikawa W, Shiratake Y, et al. A case of benign symmetric lipomatosis. Jpn J Plast Surg. 2004;47:71–77. (in Japanese) [Google Scholar]
- Umabuchi T, Umezawa Y, Ota Y, et al. Liposuction for a case of benign symmetric lipomatosis (BSL). Nishinihon J Dermatol. 2004;66:482–484. (in Japanese) [Google Scholar]
- Sugino H, Aoki R Mesotherapy and injection lipolysis. PEPARS. 2010;45:33–41. [Google Scholar]
- Carlin MC, Ratz JL. Multiple symmetric lipomatosis: treatment with liposuction. J Am Acad Dermatol. 1988;18(2, Part 1):359–362. [PubMed] [Google Scholar]
- Sato M, Hujiwara S, Ikeda T, et al. A case of benign symmetric lipomatosis. Rinsho Derma (Tokyo) 2011;53:1058–1061. (in Japanese) [Google Scholar]
Articles from Plastic and Reconstructive Surgery Global Open are provided here courtesy of Wolters Kluwer Health
Copyright
Copyright © 2015 The Authors. Published by Wolters Kluwer Health, Inc. on behalf of The American Society of Plastic Surgeons. All rights reserved.This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License, where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially.