Primary Cardiac Undifferentiated High-Grade Intimal Pleomorphic Sarcoma
Introduction
Primary cardiac sarcomas (PCSs) are extremely rare with only a few cases reported in the literature. About 25% of primary cardiac tumors are malignant, and of those 75% are sarcomas [1]. Radiologic similarities to benign myxomas/thrombus make PCSs a diagnostic challenge. Clinical presentations of PCSs include cerebrovascular accident, pulmonary embolism (PE), valvular dysfunctions, arrhythmias, and congestive heart failure. Imaging modalities such as transthoracic echocardiogram (TTE), transesophageal echocardiogram (TEE), cardiovascular magnetic resonance imaging (CMR), positron emission tomography (PET), and computed tomography (CT) can provide initial information about the tumor location, size and the need for surgery. Chemotherapy and immunotherapy are based on histologic subtype of the tumor. Here we report two cases of undifferentiated PCSs, its diagnostic dilemmas and therapeutic challenges.
Case Reports
Case 1
A 79-year-old female with past medical history of hypertension and hyperlipidemia presented with progressively worsening dyspnea on exertion and dry cough for 1 month. Electrocardiogram (ECG) showed normal sinus rhythm and left axis deviation. TTE revealed a large mobile echodensity in the right ventricular outflow tract (RVOT) measuring 6 × 2 cm (Fig. 1a, b). The peak RVOT velocity was elevated at 4.2 m/s, consistent with significant RVOT obstruction. The right ventricle was mildly enlarged and hypokinetic. CT angiogram of the chest showed intraluminal mass in the RVOT extending into the right pulmonary artery, with smaller filling defects in the distal segmental branches (Fig. 2a, b).

Case 1: TTE demonstrating large mobile, well circumscribed echo-density in the right ventricular outflow tract (RVOT) measuring 6 × 2 cm. TTE: transthoracic echocardiogram.
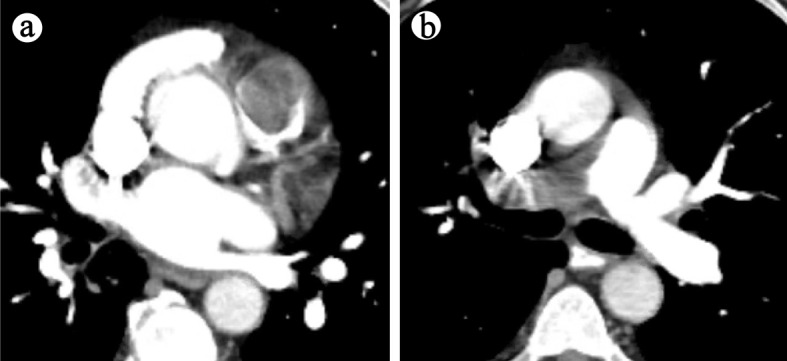
(a) Case 1: CT angiogram demonstrating large intraluminal mass centered in the RVOT. (b) Large eccentric mural thrombus in right main pulmonary artery with smaller filling defects in the distal segmental branches. CT: computed tomography; RVOT: right ventricular outflow tract.
Differential diagnosis
Based on the clinical scenario, pulmonary thromboembolism was a possibility, and the patient was started on heparin infusion. However, the patient’s dyspnea on exertion could also have been attributed to RVOT obstruction which is rarely reported in the setting of PE. Furthermore, the well circumscribed appearance of the mass on TTE was more characteristic of a tumor. In addition, the right ventricular remodeling with global hypokinesis was consistent with right ventricular pressure overload rather than the characteristic McConnell’s sign seen in PE.
Diagnostic workup/interventions
Further workup included a cardiac magnetic resonance imaging (MRI) which showed an enhancing RVOT mass concerning for sarcoma or other malignancies. PET scan revealed these lesions to be hypermetabolic, increasing suspicion for malignancy. The decision was made for surgical resection of the mass. The patient underwent an incomplete surgical resection of the cardiac mass with positive tumor margins. Pathology confirmed undifferentiated intimal pleomorphic sarcoma with 90% tumor infiltrating immune cells positive for programmed death-ligand 1 (PD-L1). Postoperative complications included cardiogenic shock and acute kidney injury from which patient recovered and underwent physical rehabilitation. She was started on immunotherapy with pembrolizumab to target PD-L1+ tumor cells.
Patient outcome
Although the patient was clinically improving, a 4-month follow-up of chest CT revealed a new solid 12 mm right suprahilar pulmonary nodule concerning for metastatic disease. The decision was made to monitor the patient clinically with continued course of pembrolizumab immunotherapy and interval follow-up imaging. Further advancement in her disease or symptomatology would require consideration for a multidisciplinary treatment approach including surgical resection if appropriate, combined with chemotherapy and/or radiation therapy.
Case 2
A 55-year-old female with past medical history of hypertension presented with left-sided weakness after sustaining a fall. Physical examination revealed decreased motor strength and sensation on the left side. ECG showed new evidence of atrial fibrillation. CT head and MRI head confirmed a right frontal lobe ischemic stroke. Evaluation for the source of embolism included a TTE which demonstrated a 2.1 × 1.2 cm mass attached to the intraatrial septum just adjacent to the anterior mitral annulus (Fig. 3a).

(a) Case 2: TTE demonstrating mass attached to the intraatrial septum adjacent to anterior mitral annulus. (b) Atrial tumor cross section. (c) Pleomorphic, spindle-shaped cells with hyper-chromatic nuclei and prominent mitotic figures. TTE: transthoracic echocardiogram.
Differential diagnosis
Although the location was atypical, a presumptive diagnosis of left atrial myxoma was made. Myxomas are the most common benign cardiac tumors typically affecting middle aged women. It can occur in either atria but are most commonly attached to the fossa ovalis of the left atrium.
Diagnostic workup/interventions
The decision was made for surgical excision of the mass. The patient underwent resection of the mass with a bovine atrial patch repair. Pathology revealed pleomorphic, spindle-shaped cells with hyperchromatic nuclei and prominent mitotic figures consistent with high-grade intimal pleomorphic sarcoma with positive tumor margins (Fig. 3b, c). Immunophenotyping was positive for murine double minute 2 (MDM2) amplification. The patient underwent local radiotherapy with CyberKnife procedure given the positive tumor margin and no metastatic disease. She was followed-up closely with serial PET/CT and TTE every 3 months.
Patient outcome
Unfortunately, 20 months later the patient presented with small bowel obstruction and pathologic right femur fracture secondary to metastases. Pathology of metastatic lesions were consistent with initial intimal tumor. TEE, CMR and PET/CT revealed recurrence of tumor in the left atrium (Fig. 4a-d). The patient was started on palliative chemotherapy with doxorubicin and olaratumab to target local tumor recurrence and metastasis. Unfortunately, the patient expired 3 years after the initial diagnosis.

(a) Case 2: TEE demonstrating recurrence of mobile heterogenous echodense mass in left atrium at 20-month interval. (b) Hypermetabolic left atrial lesion on PET/CT. (c) Mass adjacent to anterior mitral leaflet (and prolapses into left ventricle) on CMR. (d) Mass within the left atrium on CMR. TEE: transesophageal echocardiogram; PET/CT: positron emission tomography/computed tomography; CMR: cardiovascular magnetic resonance imaging.
Source: https://www.ncbi.nlm.nih.gov/pmc/