Impact of childhood burn injuries on breastfeeding
Case presentation
In May 2015, a 20 year old first-time mother at 36 weeks gestation was seen in a district health clinic in Kuching, Sarawak in regards to her ability to breastfeed. She had a history of a flame burn at the age of 5 years old to her chest, abdomen, upper limb and part of her trunk. A skin graft was done on her whole chest and abdomen. Despite the injuries, she had pubertal and antenatal breast development. Her abdomen was able to stretch to accommodate her pregnancy. Physical examination showed a pregnancy which corresponded to date. The skin over her chest and abdomen appeared tight with areas of hyperpigmentation and hypopigmentation due to scarring from the skin graft. Breast tissues were palpable over her chest. The areola and nipple tissue were completely absent with complete scarring of the nipple-areolar complex. There was no duct opening to the areola for milk expression or leakage. Counselling regarding her breastfeeding issues was done. She delivered her baby at full term via spontaneous vaginal delivery with no complication. Oral cabergoline 1 mg was given on the first day postpartum. The baby was given infant formula via bottle feeding as the feeding method of choice.
Case report
A young first time mother at 36 weeks period of gestation was seen in a health clinic in Kuching, Sarawak with regards to her ability to breastfeed. She was referred from a clinic in a small district located around 31 km from the nearest tertiary hospital. She had history of a flame burn at the age of 5 years old to her chest, abdomen, upper limb and part of her trunk. She was admitted for about 4 months in the Burn Unit in a tertiary hospital where skin grafts were done in 3 stages on her whole chest and abdomen. Despite the injuries, she noticed pubertal breasts development. During this pregnancy, she had further breast development which increased in size and her abdomen was able to stretch to accommodate her pregnancy. Physical examination showed a pregnancy which corresponded to her date. The skin over her chest and abdomen appeared tight with areas of hyperpigmentation and hypopigmentation due to scarring from the skin graft. There were normal breasts swelling and breast tissues palpable over her chest with the absence of areola and nipple. Sensations over the skin grafted area were intact. The breasts and abdomen (antenatally) are shown in Fig. 1 (Antenatal: Right breast), Fig. 2 (Antenatal: Left breast) and Fig. 3 (Antenatal: Breasts and abdomen).

Antenatal: Right breast
Antenatal: Left breast
Antenatal: Breasts and abdomen
Management
A counselling session was conducted to explore her expectations and hopes regarding her ability to breastfeed her baby. Further counselling was done to prepare her that she might not be able to breastfeed her child due to her physical condition and may need lactation suppression post-birth. Alternative methods of feeding were discussed.
She birthed her infant at 36 weeks and 5 days via spontaneous vaginal delivery without any complications. Oral cabergoline 1 mg was given on the first postpartum day to suppress lactation. The baby was given infant formula via bottle feeding as the feeding method of choice. On subsequent days, she noticed her breasts reduced in size.
At day 6 postpartum, her breasts reduced in size almost to the pre-pregnancy stage as shown in Fig. 4 (Postnatal Day 6: Breasts).

Postnatal Day 6: Breasts
A breast ultrasound was done at day 6 postpartum. It showed dilated lactiferous ducts at retroareolar region bilaterally, consistent with lactating ducts of the breasts. The normally appearing vague shadow of the nipple was not seen. However, the tightly packed ducts seen parallel to the ultrasound beam are suggestive of major ducts to the possible location of the nipple as shown in Fig. 5 (Ultrasound: Right breast) and Fig. 6 (Ultrasound: Left breast).
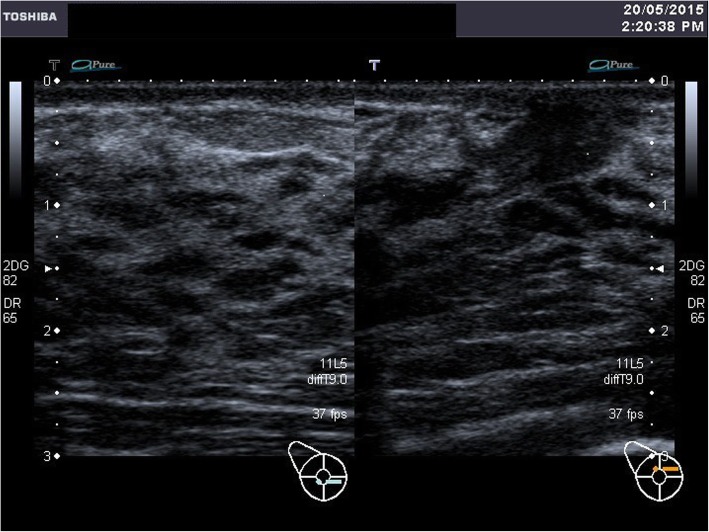
Ultrasound: Right breast
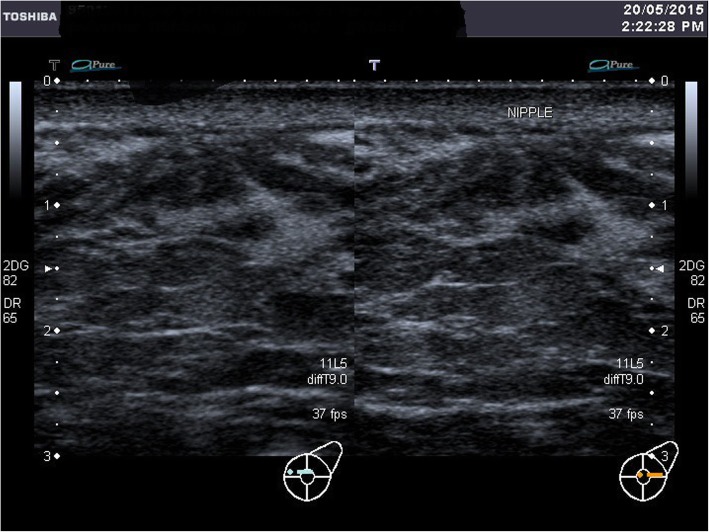
Ultrasound: Left breast
A discussion with the plastic surgeon was made regarding the possibility of surgery to enable her to breastfeed in her future pregnancies. However, patient was not keen for any surgeries as she was made aware of the risks and complications. She also felt contented with her decision to bottle feed her child with infant formula.
Scheduled home postnatal visits were done to ensure that mother and baby were coping well. She had fully accepted that she was not able to breastfeed her child due to her physical limitations. Her husband and family were very understanding and supportive towards her. The baby was doing well with infant formula feeding. There were no signs and symptoms of postpartum depression.
Author information
1Department of Family Medicine, Faculty of Medicine and Health Sciences, Universiti Malaysia Sarawak, Kota Samarahan, Sarawak Malaysia
2Department of Family Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Selangor Malaysia
3Department of Radiology, Faculty of Medicine and Health Sciences, Universiti Malaysia Sarawak, Kota Samarahan, Sarawak Malaysia